Welcome to our article series on the fascinating topic of angiogenesis in wound healing. In this series, we will explore the intricate mechanisms of angiogenesis and its crucial role in promoting tissue regeneration during the wound healing process.
Wound healing is a complex biological process that involves various stages and cellular responses. Angiogenesis, the formation of new blood vessels, plays a vital role in each phase of wound healing, from inflammation to proliferation and remodeling.
As we delve deeper into this subject, we will examine the relationship between angiogenesis, oxygen supply, collagen production, and cell migration in the context of wound healing. We will also discuss the influence of growth factors and therapeutic approaches that target angiogenesis to enhance healing outcomes.
Key Takeaways:
- Angiogenesis is the formation of new blood vessels and is crucial for wound healing and tissue regeneration.
- Oxygen supply facilitated by angiogenesis plays a vital role in providing the necessary resources for wound healing.
- Growth factors regulate the process of angiogenesis and contribute to the overall healing process.
- Angiogenesis promotes collagen production, which is essential for tissue repair and regeneration.
- Cell migration guided by angiogenic blood vessels aids in the wound healing process.
What is Angiogenesis?
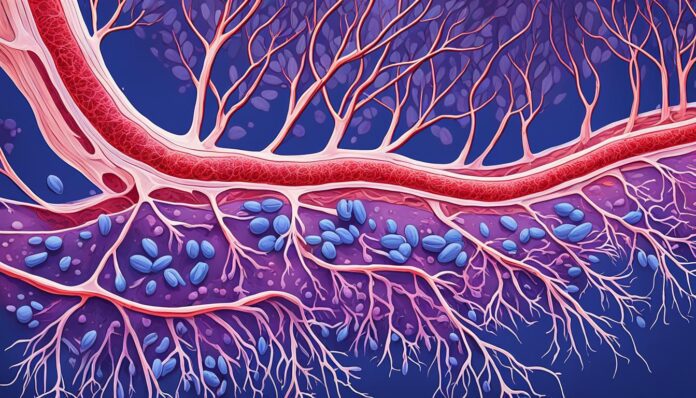
Angiogenesis is the process of blood vessel formation, crucial for various physiological and pathological conditions, including wound healing. It involves the sprouting and growth of new blood vessels from pre-existing ones, enabling the delivery of oxygen and nutrients to tissues.
During wound healing, angiogenesis plays a vital role in restoring blood supply to the injured area, promoting tissue regeneration. When a wound occurs, the body initiates a complex cascade of events to repair the damaged tissue. Angiogenesis is a key component of this process, as it facilitates the formation of a new vascular network within the wound bed.
The formation of new blood vessels involves a series of sequential steps, including endothelial cell proliferation, migration, and tube formation. It is regulated by a delicate balance of pro-angiogenic and anti-angiogenic factors in the wound microenvironment.
Angiogenesis begins with the degradation of the existing extracellular matrix and basement membrane surrounding blood vessels. This allows endothelial cells to migrate towards the wound bed and form new blood vessel sprouts. These sprouts eventually connect and develop into functional blood vessels, enhancing blood flow and promoting wound healing.
Understanding angiogenesis is essential for comprehending how blood vessel formation contributes to the healing of wounds.
| Key Points: |
|---|
| Angiogenesis is the process of blood vessel formation |
| It plays a crucial role in wound healing |
| Angiogenesis involves the sprouting and growth of new blood vessels from pre-existing ones |
| It facilitates the delivery of oxygen and nutrients to tissues |
The Phases of Wound Healing
Wound healing is a complex process that involves several phases, each playing a crucial role in the restoration of tissue integrity. Understanding these phases is essential for comprehending the significance of angiogenesis in promoting effective wound healing.
Inflammation
The first phase of wound healing is inflammation, which begins immediately after injury. In this phase, injured blood vessels constrict to minimize bleeding, followed by blood clot formation to prevent the entry of pathogens. The release of inflammatory mediators, such as cytokines and growth factors, initiates the recruitment of immune cells and the removal of debris.
Proliferation
During the proliferation phase, new tissue is generated to replace the damaged or lost tissue. Fibroblasts, a type of cell present in connective tissue, migrate to the wound site and produce collagen, a key protein in wound healing. Concurrently, endothelial cells, which line blood vessels, undergo angiogenesis to form new capillaries that supply oxygen and nutrients to the developing tissue.
Remodeling
The final phase of wound healing is remodeling, wherein the newly formed tissue undergoes maturation and organization. During this phase, excessive collagen is removed, and the tissue gains strength through the cross-linking of collagen fibers. The remodeling phase can last for several months, as the wound gradually transitions to a scar.
Throughout the wound healing process, angiogenesis plays a vital role, facilitating the delivery of oxygen and nutrients required for cell proliferation and tissue regeneration. The formation of new blood vessels ensures an adequate blood supply to the healing wound, promoting optimal healing outcomes.
Angiogenesis and Oxygen Supply in Wound Healing
One critical aspect of wound healing is the supply of oxygen to the wound site, and angiogenesis plays a crucial role in this process. Angiogenesis, the formation of new blood vessels, helps ensure an adequate oxygen supply to support the healing process and promote tissue regeneration.
When a wound occurs, the body initiates a series of healing responses, including inflammation and the release of growth factors. These growth factors stimulate angiogenesis, triggering the formation of new blood vessels. The newly formed blood vessels then supply oxygen and essential nutrients to the wound, facilitating the healing process.
Oxygen supply by angiogenesis
By delivering oxygen, angiogenesis creates an optimal environment for healing. Oxygen is essential for cell metabolism and plays a vital role in various cellular processes involved in wound repair, such as collagen synthesis and cell proliferation. Adequate oxygen supply promotes the growth of new tissue, allowing the wound to close and heal effectively.
Research has shown that impaired angiogenesis can significantly impact wound healing outcomes. Conditions that restrict oxygen supply, such as chronic inflammation or impaired vascularity, can delay or inhibit the healing process. Therefore, promoting angiogenesis is crucial to ensure an adequate oxygen supply and enhance wound healing.
Here is a table illustrating the relationship between angiogenesis and oxygen supply in wound healing:
| Factors | Impact on Oxygen Supply |
|---|---|
| Inflammation | Can compromise blood flow and oxygen delivery to the wound site. |
| Impaired Vascularization | Restricts the formation of new blood vessels, leading to inadequate oxygen supply. |
| Hypoxia | Oxygen deficiency hinders wound healing and impairs angiogenesis. |
| Chronic Diseases | Conditions like diabetes and cardiovascular disease can impair angiogenesis and oxygen supply. |
Ensuring optimal angiogenesis and oxygen supply is crucial for effective wound healing. In the next section, we will explore the role of growth factors in regulating angiogenesis and how they contribute to the healing process.
Growth Factors and Angiogenesis
In the complex process of wound healing, growth factors play a crucial role in regulating angiogenesis. These signaling molecules act as powerful messengers, orchestrating the intricate dance between cells, tissues, and blood vessels.
Growth factors are secreted by various cells in the body, including platelets, fibroblasts, and macrophages. They act locally to stimulate angiogenesis, promoting the growth of new blood vessels from pre-existing ones.
One of the key growth factors involved in angiogenesis is vascular endothelial growth factor (VEGF). It plays a central role in both physiological and pathological angiogenesis, including wound healing processes.
Role of Growth Factors in Angiogenesis
Growth factors exert their effects on angiogenesis through multiple mechanisms:
- Induction of endothelial cell proliferation: Growth factors stimulate the reproduction and division of endothelial cells, the building blocks of blood vessels.
- Promotion of endothelial cell migration: Growth factors guide endothelial cells to migrate towards the site of angiogenesis, ensuring the formation of new blood vessels.
- Regulation of vessel permeability: Growth factors modulate the permeability of blood vessels, allowing easy passage of oxygen, nutrients, and immune cells to support the healing process.
- Initiation of angiogenic sprouting: Growth factors initiate the sprouting process, where new blood vessels extend from existing ones to reach the wounds.
By influencing these processes, growth factors promote the intricate network of blood vessels necessary for successful wound healing. The regulated formation of new blood vessels ensures an adequate supply of oxygen and nutrients to the wound site, facilitating tissue regeneration and recovery.
| Growth Factors | Role in Angiogenesis |
|---|---|
| Vascular Endothelial Growth Factor (VEGF) | Stimulates endothelial cell proliferation and migration, enhances vessel permeability, and promotes angiogenic sprouting |
| Platelet-Derived Growth Factors (PDGF) | Promotes the recruitment and proliferation of smooth muscle cells and fibroblasts, aiding in the maturation and stabilization of new blood vessels |
| Fibroblast Growth Factors (FGF) | Induces endothelial cell proliferation, migration, and survival, playing a crucial role in early angiogenesis |
As illustrated in the table, various growth factors contribute to the regulation of angiogenesis during wound healing.
Understanding the interactions between growth factors and angiogenesis provides valuable insights into potential therapeutic approaches for enhancing wound healing. By manipulating the activity of specific growth factors, researchers and medical professionals aim to optimize healing outcomes and improve patient well-being.
Angiogenesis and Collagen Production
In the intricate process of wound healing, angiogenesis plays a vital role in promoting collagen production, which is essential for tissue regeneration. Collagen, the most abundant protein in the human body, provides structural support to various tissues and helps in the formation of scar tissue.
When a wound occurs, the body initiates a series of events, including inflammation and angiogenesis, to repair and restore the damaged tissue. Angiogenesis brings oxygen and nutrients to the wound site, creating an optimal environment for collagen synthesis.
During angiogenesis, endothelial cells proliferate and migrate towards the wound, forming new capillary loops. These blood vessels provide access to oxygen and growth factors needed to stimulate fibroblasts, the cells responsible for collagen production. Angiogenesis and collagen synthesis go hand in hand, ensuring the proper healing of wounds.
Collagen production is crucial for wound healing as it contributes to the strength and integrity of the repaired tissue. It provides a scaffold for cell migration and supports the formation of granulation tissue, which eventually forms the scar. Additionally, collagen helps modulate the inflammatory response and provides a barrier against infection.
The interplay between angiogenesis and collagen production highlights the importance of both processes in effective wound healing. By ensuring an adequate blood supply and stimulating fibroblasts, angiogenesis promotes the synthesis of collagen, facilitating the formation of new, healthy tissue.
The Impact of Angiogenesis on Collagen Production
To understand the impact of angiogenesis on collagen production, it is helpful to examine the stages involved in collagen synthesis during wound healing:
- Phase 1 – Inflammation: In the initial inflammatory phase, angiogenesis begins, bringing in immune cells and growth factors. These factors stimulate fibroblast activation and collagen synthesis.
- Phase 2 – Proliferation: During this phase, fibroblasts multiply and migrate towards the wound site. Angiogenic blood vessels provide the necessary oxygen and nutrients for collagen production.
- Phase 3 – Remodeling: The final phase involves the remodeling of collagen fibers, aligning them to provide strength to the repaired tissue. Angiogenesis continues to support this process by maintaining adequate blood supply.
As angiogenesis progresses through these phases, collagen production is enhanced, enabling the formation of a strong and functional tissue matrix. The coordination between angiogenesis and collagen synthesis is crucial for successful wound healing and optimal tissue regeneration.
| Angiogenesis and Collagen Production: Key Takeaways |
|---|
| Angiogenesis promotes collagen production during wound healing. |
| Newly formed blood vessels deliver oxygen and nutrients necessary for fibroblast activation and collagen synthesis. |
| Collagen provides structural support, guides cell migration, and promotes the formation of granulation tissue. |
| Angiogenesis and collagen production are interdependent processes crucial for effective tissue regeneration. |
Angiogenesis and Cell Migration
During the process of wound healing, cell migration plays a crucial role in tissue repair. Angiogenesis is closely intertwined with cell migration, facilitating the recruitment of cells to the site of injury.
Angiogenic blood vessels provide a pathway for different cell types, such as fibroblasts and immune cells, to migrate towards the wound site. These migrating cells contribute to the formation of granulation tissue, which is essential for wound closure and tissue regeneration. The guidance cues provided by angiogenic blood vessels help direct cell migration, ensuring their presence at the site of injury for efficient wound healing.
The Role of Angiogenesis in Cell Migration
Angiogenesis not only serves as a means of delivering oxygen and nutrients to the wound but also acts as a navigational system for cells to migrate towards the damaged area. As angiogenic blood vessels extend into the wound bed, they release signaling molecules that attract and guide migrating cells. These cues promote the directional movement of cells, allowing them to reach the wound site and participate in the healing process.
Furthermore, angiogenesis promotes the formation of a network of blood vessels that create a structurally supportive environment for migrating cells. This vascular network provides a scaffold for cells to anchor and move along, enhancing their ability to reach the wound and contribute to tissue repair. The synchronized interplay between angiogenesis and cell migration is vital for achieving efficient wound healing and optimal tissue regeneration.
Targeting Angiogenesis and Cell Migration for Enhanced Wound Healing
Understanding the relationship between angiogenesis and cell migration opens up new avenues for therapeutic interventions in wound healing. By modulating angiogenesis, researchers can influence the guidance cues provided by angiogenic blood vessels, ultimately enhancing cell migration to the wound site. Strategies aimed at promoting angiogenesis and facilitating cell migration include the use of growth factors, bioactive molecules, and tissue engineering approaches.
Advancements in our understanding of the cellular and molecular mechanisms underlying angiogenesis and cell migration hold great promise for developing targeted therapies. By harnessing the power of these processes, researchers can pave the way for innovative treatments that accelerate wound healing, minimize scarring, and promote tissue regeneration.
| Role of Angiogenesis and Cell Migration in Wound Healing | Benefits |
|---|---|
| Promotes recruitment of cells to the wound site | Enhances tissue repair |
| Guides migrating cells towards the damaged area | Facilitates wound closure |
| Provides a navigational system for efficient cell movement | Accelerates wound healing |
| Creates a supportive vascular network for cells | Optimizes tissue regeneration |
Therapeutic Approaches Targeting Angiogenesis
In the pursuit of enhancing wound healing, various therapeutic approaches have emerged to target angiogenesis. These strategies aim to promote the formation of new blood vessels and optimize the process of tissue regeneration. One of the key methods employed is the use of growth factors.
Growth factors play a crucial role in stimulating angiogenesis and facilitating wound healing. They act as signaling molecules that initiate the formation of new blood vessels, promoting the delivery of oxygen and nutrients to the wounded area. By harnessing the power of growth factors, clinicians can enhance angiogenesis and accelerate the healing process.
Another therapeutic approach is the utilization of bioactive molecules. These molecules are designed to mimic the natural cues present during angiogenesis, thereby promoting the growth of new blood vessels. By administering bioactive molecules, clinicians can stimulate angiogenesis in non-healing wounds and foster an optimal environment for tissue regeneration.
Beyond growth factors and bioactive molecules, other strategies targeting angiogenesis show promise in wound healing. These include the use of scaffolds, gene therapy, and stem cells to promote angiogenesis and facilitate tissue repair. Researchers continue to explore innovative therapeutic approaches that optimize angiogenesis to improve wound healing outcomes.
Through the intervention of therapeutic approaches targeting angiogenesis, remarkable advancements have been made in the field of wound healing. These approaches provide new avenues for clinicians and researchers to enhance the body’s natural healing processes and overcome challenges associated with impaired wound healing.
Next, we will explore the factors that can positively or negatively influence angiogenesis in wound healing. Understanding these factors is essential in developing effective treatment strategies that harness the full potential of angiogenesis for improved wound recovery.
Factors Affecting Angiogenesis in Wound Healing
Angiogenesis plays a critical role in wound healing and tissue regeneration. However, several factors can influence angiogenesis in both positive and negative ways. Understanding these factors is crucial in designing effective therapeutic interventions for promoting successful wound healing.
The Impact of Age
Age is known to affect angiogenesis in wound healing. As individuals age, the angiogenic response may be impaired, leading to delayed wound healing and compromised tissue regeneration. Studies have shown that older individuals may have decreased levels of angiogenic factors, such as vascular endothelial growth factor (VEGF), which is essential for stimulating the formation of new blood vessels.
The Influence of Diabetes
Diabetes can have a significant impact on angiogenesis in wound healing. High blood sugar levels and impaired circulation associated with diabetes can inhibit the formation of new blood vessels, leading to poor wound healing outcomes. Additionally, diabetes-related complications, such as neuropathy and poor oxygen supply, further exacerbate the impaired angiogenic response.
The Effects of Smoking
Smoking has been shown to negatively affect angiogenesis in wound healing. The toxic components in cigarette smoke can disrupt the delicate balance of angiogenic factors, impairing the formation of new blood vessels. Smoking also reduces oxygen delivery to the wound site, further compromising the healing process. Quitting smoking is crucial to promote optimal angiogenesis and enhance wound healing.
Other Factors Affecting Angiogenesis
Various other factors can influence angiogenesis in wound healing. Chronic diseases, such as cardiovascular disease or hypertension, can perturb the angiogenic process and impede efficient tissue regeneration. Inflammatory conditions, such as rheumatoid arthritis or chronic infections, can also disrupt angiogenesis and hinder wound healing. Moreover, the use of certain medications, such as corticosteroids or anti-inflammatory drugs, may affect angiogenesis.
Understanding the factors that can positively or negatively impact angiogenesis in wound healing is critical in developing targeted therapeutic approaches. By addressing these factors and promoting optimal angiogenesis, healthcare professionals can enhance the outcomes of wound healing and promote successful tissue regeneration.
Advances in Angiogenesis Research
In recent years, significant advances have been made in angiogenesis research, paving the way for exciting developments in the field of wound healing and tissue engineering. These advancements hold great promise for improving the outcomes of patients with chronic wounds and promoting efficient tissue regeneration.
Exploring Tissue Engineering Techniques
Tissue engineering has emerged as a groundbreaking approach in wound healing, harnessing the potential of angiogenesis to accelerate the regeneration process. Researchers have developed innovative methods to engineer scaffolds and matrices that provide structural support and facilitate the formation of new blood vessels within the wound site. These tissue-engineered constructs enhance angiogenesis and promote efficient wound healing.
Novel Therapies Harnessing Angiogenesis
New therapeutic strategies that specifically target angiogenesis have been developed to enhance wound healing. These therapies utilize growth factors, bioactive molecules, and gene therapy to stimulate angiogenesis and promote the formation of new blood vessels. By targeting the underlying mechanisms of angiogenesis, these innovative interventions offer a potential solution for patients with impaired wound healing.
The Potential of Regenerative Medicine
Regenerative medicine, a rapidly evolving field, seeks to restore damaged tissues and organs by harnessing the body’s innate healing potential. Researchers are investigating the use of stem cells, biomaterials, and growth factors to stimulate angiogenesis and promote tissue regeneration. These cutting-edge approaches hold immense potential for revolutionizing wound healing and improving patient outcomes.
Emerging Technologies
Advances in angiogenesis research have also led to the development of novel technologies that enhance our understanding of this complex process. Advanced imaging techniques, such as confocal microscopy and nanoparticle-based imaging, enable researchers to visualize and study angiogenesis in unprecedented detail. These technological advancements provide valuable insights into the dynamic nature of angiogenesis during wound healing.
The future of angiogenesis research in wound healing
As research in angiogenesis continues to progress, it is likely that further advancements will be made in the field of wound healing. By harnessing the power of angiogenesis, scientists and healthcare professionals have the potential to revolutionize the treatment of chronic wounds and significantly improve patient outcomes. However, challenges such as scalability, cost-effectiveness, and regulatory approval still need to be addressed to fully translate these research findings into clinical practice.
Future Directions and Challenges
As research in the field of angiogenesis and wound healing continues to evolve, several future directions and challenges emerge. These areas of focus and obstacles aim to advance our understanding and improve therapeutic interventions targeting angiogenesis.
1. Harnessing Nanotechnology
One promising avenue for future research involves the integration of nanotechnology in angiogenesis and wound healing. Nanomaterials can be engineered to deliver growth factors, promote angiogenesis, and enhance wound healing outcomes. By leveraging the unique properties of nanoparticles, researchers can develop innovative strategies to optimize the angiogenic process.
2. Tailoring Therapies for Specific Wound Types
Another future direction is the development of personalized therapies that target specific wound types. Understanding the distinct angiogenic mechanisms underlying acute wounds, chronic wounds, and burns can guide the design of tailored treatment approaches. By addressing the specific challenges posed by different wound types, researchers can optimize angiogenesis-based therapies for improved clinical outcomes.
3. Enhancing Tissue Engineering Techniques
Advancing tissue engineering techniques is another area of focus in the future of angiogenesis research. Combining angiogenic materials, such as bioactive scaffolds and growth factors, with regenerative cells holds immense potential for promoting angiogenesis and tissue regeneration. Innovations in biomimetic scaffolds and 3D printing technologies can further enhance the architecture and functionality of engineered tissues.
4. Addressing Hurdles in Clinical Translation
While significant progress has been made in angiogenesis research, there are still challenges to overcome in translating these findings into clinical practice. One obstacle is the need for standardized protocols and guidelines for angiogenesis-based therapies. Additionally, cost-effective production methods for growth factors and other therapeutic agents must be developed to ensure widespread accessibility.
5. Unraveling the Role of Microenvironment Factors
The microenvironment surrounding wounds plays a crucial role in angiogenesis and wound healing. Investigating the influence of factors such as mechanical forces, extracellular matrix components, and immune cells on angiogenesis can provide valuable insights for future interventions. Understanding how these factors interact with angiogenesis will enable the development of targeted therapies that optimize the wound healing process.
These future directions and challenges indicate the vast potential for advancements in the field of angiogenesis and wound healing. By addressing these research areas and overcoming obstacles, we can pave the way for more effective and personalized treatment options, ultimately improving outcomes for patients with impaired wound healing.
Conclusion
Angiogenesis plays a pivotal role in wound healing, promoting tissue regeneration and recovery. Throughout this article, we have explored the intricate process of angiogenesis and its significance in the healing of wounds. By facilitating the formation of new blood vessels, angiogenesis ensures an adequate oxygen supply and the delivery of essential nutrients to the wound site.
The importance of angiogenesis in wound healing cannot be overstated. It not only supports the growth and migration of cells necessary for repair but also stimulates collagen production, a critical component of tissue regeneration. Additionally, angiogenesis is closely intertwined with the action of growth factors that regulate this process, further enhancing wound healing outcomes.
However, there is still much to learn and discover about angiogenesis in the context of wound healing. Further research is needed to explore innovative therapeutic approaches and overcome the challenges associated with enhancing angiogenesis. These advancements have the potential to revolutionize wound healing strategies and pave the way for improved clinical outcomes in patients with chronic and non-healing wounds.