Lynch Syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC), is a genetic condition that increases the risk of various cancers, especially colorectal cancer. This disorder is caused by mutations in DNA mismatch repair genes like MLH1, MSH2, MSH6, and PMS2, leading to a higher likelihood of DNA errors during cell division.
Individuals with this syndrome are more likely to develop colorectal cancer and other cancers, such as endometrial, ovarian, and gastric cancer, often at a younger age.
Early diagnosis and regular screening are essential for managing Lynch Syndrome. Genetic testing and counseling help identify at-risk individuals and guide preventive measures and treatments. This blog post will explore Lynch Syndrome, its genetic basis, associated cancer risks, and strategies for prevention and management.
What is Lynch Syndrome?
Definition of Lynch Syndrome
Lynch Syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC), is an inherited disorder that increases the risk of various cancers. Unlike other hereditary cancer syndromes, Lynch Syndrome does not typically involve the formation of numerous polyps in the colon. Instead, individuals with Lynch Syndrome are prone to developing cancers, often at a younger age than the general population.
Overview of DNA mismatch repair (MMR)
At the heart of Lynch Syndrome is a defect in the DNA mismatch repair (MMR) system. The MMR system is responsible for correcting errors that occur during DNA replication. When this system fails, these errors accumulate, leading to genetic instability and an increased risk of cancer.
Common mutations involved
The most common genetic mutations associated with Lynch Syndrome occur in the MLH1, MSH2, MSH6, and PMS2 genes. These genes produce proteins crucial for the MMR process. Mutations in any of these genes can impair the MMR system, allowing errors to persist in the DNA, which can ultimately lead to cancer development. Identifying these mutations through genetic testing can help at-risk individuals take preventive measures to manage their cancer risk effectively.
Genetic Testing and Diagnosis of Lynch Syndrome
Importance of genetic testing for Lynch Syndrome
Genetic testing is a critical tool for identifying individuals with Lynch Syndrome. Early detection through genetic testing allows for proactive management of cancer risk, which can significantly improve outcomes. Testing typically analyzes a blood sample to detect mutations in the MLH1, MSH2, MSH6, and PMS2 genes, which are known to be associated with Lynch Syndrome.
Genetic counseling and its role in diagnosis
Genetic counseling plays a vital role in the diagnostic process. A genetic counselor can help individuals understand the implications of their test results, including their risk of developing Lynch Syndrome-associated cancers. Counselors also provide guidance on the appropriate next steps, which might include regular surveillance, preventive measures, or informing at-risk family members.
Screening tests: Microsatellite instability (MSI) and Immunohistochemistry (IHC)
Screening tests such as Microsatellite Instability (MSI) and Immunohistochemistry (IHC) are also used in the diagnostic process. MSI testing examines the DNA from tumor tissue to detect abnormalities that suggest a defect in the mismatch repair system. IHC testing looks for the presence or absence of the MMR proteins in the tumor tissue. The absence of these proteins can indicate a potential mutation in the corresponding MMR gene, prompting further genetic testing. These screening tests are essential for confirming the diagnosis of Lynch Syndrome and guiding treatment and management strategies.
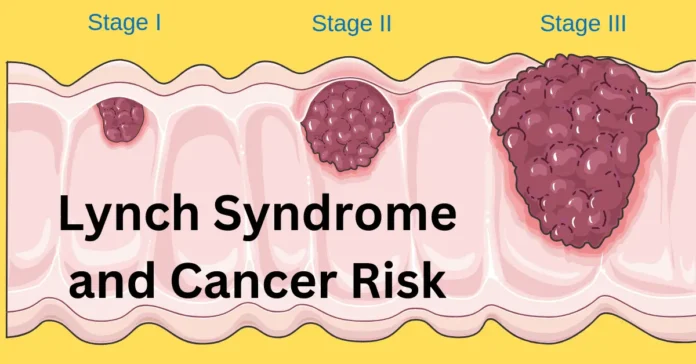
Cancer Risks Associated with Lynch Syndrome
Increased risk of colorectal cancer
Individuals with Lynch Condition face a significantly elevated risk of developing several types of cancer compared to the general population. The most prominent among these is colorectal cancer. Those with Lynch Syndrome often develop colorectal cancer at a younger age and may have multiple occurrences over their lifetime.
Other cancers linked to Lynch condition
Beyond colorectal cancer, Lynch Syndrome is also linked to an increased risk of other cancers. Endometrial cancer is particularly common among women with this Syndrome, often serving as a primary indicator of the condition. Ovarian cancer is another significant risk, with women having a notably higher chance of developing this cancer compared to those without Lynch Syndrome. Additionally, there is an elevated risk of gastric cancer, as well as cancers of the urinary tract, small intestine, and certain types of skin cancer.
Statistics and figures related to cancer risk
Statistics highlight the gravity of these risks. For example, individuals with Lynch Syndrome have up to an 80% lifetime risk of developing colorectal cancer. The risk for endometrial cancer is around 40-60%, and for ovarian cancer, it ranges from 10-12%.
These figures underscore the importance of regular screening and vigilant monitoring for early signs of cancer in individuals with Lynch Syndrome. Proactive management, including genetic counseling and tailored surveillance strategies, can significantly improve outcomes and reduce the overall cancer burden for those affected by this genetic condition.
Preventive Measures and Early Detection
For individuals with Lynch Syndrome, preventive measures and early detection are crucial in managing their elevated cancer risk. Regular screening and surveillance are the cornerstone of these efforts, enabling early identification and treatment of cancer before it progresses.
Regular Screening and Surveillance Recommendations
Colonoscopy is the most important screening tool for those with Lynch condition, recommended to begin between ages 20-25 and to be repeated every 1-2 years. This frequent screening helps detect precancerous polyps and early-stage colorectal cancer, allowing for timely intervention.
For women, doctors recommend an endometrial biopsy starting at age 30-35 and repeating it annually to screen for endometrial cancer. Additionally, they may use transvaginal ultrasound to monitor the ovaries for signs of ovarian cancer.
Preventive Surgeries and Their Effectiveness
Preventive (prophylactic) surgeries can significantly reduce cancer risk for individuals with Lynch Syndrome. Colectomy, the surgical removal of the colon, can prevent colorectal cancer but is generally considered when multiple polyps are present or if cancer is detected.
For women, prophylactic hysterectomy (removal of the uterus) and oophorectomy (removal of the ovaries) are options to consider after childbearing is complete to prevent endometrial and ovarian cancers. These surgeries have been shown to effectively reduce the incidence of these cancers, providing peace of mind for many patients.
Lifestyle Changes to Reduce Cancer Risk
In addition to medical interventions, lifestyle changes can also play a role in reducing cancer risk for individuals with Lynch condition. Adopting a healthy diet rich in fruits, vegetables, and whole grains, along with maintaining a healthy weight, can have protective effects.
Regular physical activity and avoiding smoking are also important preventive measures. Limiting alcohol intake and reducing red and processed meat consumption may further decrease cancer risk.
By combining regular screening, considering preventive surgeries, and making healthy lifestyle choices, individuals with Lynch Syndrome can better manage their cancer risk and improve their overall health outcomes.
Managing and Living with Lynch Syndrome
Living with Lynch Syndrome requires proactive management to address the heightened cancer risks associated with the condition. A combination of early detection, treatment options, and support resources can help individuals with Lynch condition navigate their health and quality of life.
Importance of Family History and Informing Relatives
Since Lynch Syndrome is hereditary, understanding and sharing family medical history is essential for identifying other at-risk individuals. Family members of someone diagnosed with this Syndrome should undergo genetic testing to determine whether they also carry the gene mutations associated with the condition.
This information can help them make informed decisions about screening and preventive measures. Early genetic testing and counseling can enable other relatives to take proactive steps toward cancer prevention.
Support Resources
Support is a critical part of managing Lynch Syndrome. The National Comprehensive Cancer Network (NCCN) provides guidelines on screening and management, offering evidence-based recommendations for healthcare providers. The American Cancer Society (ACS) is another valuable resource, offering educational materials, support groups, and information on living with cancer.
Conclusion
Lynch Syndrome significantly increases the risk of several cancers, especially colorectal, endometrial, and ovarian cancers. Genetic testing and regular screenings are crucial for early detection, and preventive surgeries can reduce cancer risk. It’s important for individuals with this condition to share their family medical history to ensure loved ones are also screened.
Seeking genetic counseling and adhering to screening guidelines can help manage the condition effectively. By staying proactive with regular check-ups and adopting a healthy lifestyle, individuals with this Syndrome can improve their long-term health outcomes.