The JAK/STAT pathway is a crucial signaling mechanism that controls various cellular functions, including immune responses, cell growth, and apoptosis.
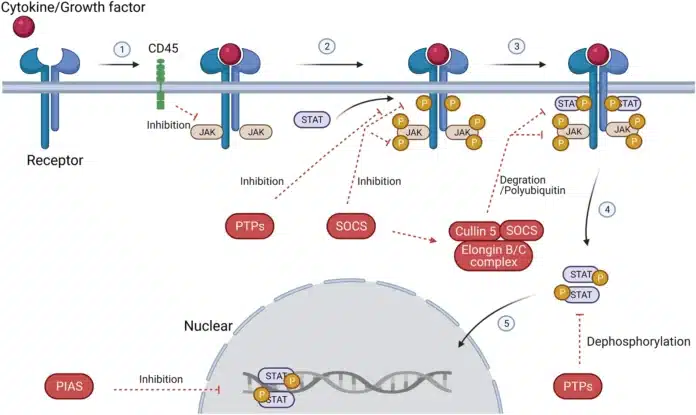
This pathway is activated when cytokines bind to specific receptors on the cell surface, triggering the activation of Janus Kinases (JAKs) and the subsequent phosphorylation of Signal Transducers and Activators of Transcription (STATs).
These activated STAT proteins then move to the cell nucleus to regulate gene expression. The JAK-STAT pathway plays an essential role in maintaining cellular homeostasis and is involved in a wide range of diseases, including cancer and autoimmune disorders.
In this blog post, we will explore the key components of the JAK-STAT pathway, its role in various diseases, and how it is targeted for therapeutic purposes, particularly in cancer treatment.
The Key Components of the JAK-STAT Pathway
The JAK-STAT pathway relies on a set of specialized proteins that work together to transmit signals from the cell surface to the nucleus. These proteins are essential for activating cellular responses to external stimuli, such as cytokines. The key components include JAK proteins, STAT proteins, and cytokine receptors. Let’s explore each of these components in detail:
JAK (Janus Kinase): Types of JAK Proteins and Their Roles
JAK proteins are a family of intracellular tyrosine kinases that play a central role in the initiation of the JAK-STAT signaling cascade. There are four members of the JAK family: JAK1, JAK2, JAK3, and TYK2. Each of these kinases is associated with specific cytokine receptors and plays distinct roles in cellular signaling.
- JAK1: Primarily involved in signaling through receptors for interferons, interleukins, and growth factors. JAK1 pairs with other JAK family members to transduce signals in various immune cells.
- JAK2: Most commonly associated with hematopoietic cytokines (e.g., erythropoietin and thrombopoietin). JAK2 is crucial for the development of blood cells and is implicated in various hematologic cancers.
- JAK3: Predominantly found in immune cells, particularly T-cells and B-cells. JAK3 is often involved in cytokine signaling related to immune responses and inflammation.
- TYK2: Works in parallel with JAK1 in certain cytokine signaling pathways, particularly those involving type I interferons and interleukins.
JAKs function by phosphorylating specific tyrosine residues on the receptor after cytokine binding. This phosphorylation event creates docking sites for STAT proteins, thereby initiating the downstream signaling process.
STAT (Signal Transducers and Activators of Transcription): Different STAT Proteins and Their Activation
STAT proteins are a family of transcription factors that mediate the effects of the JAK-STAT pathway. The main STAT proteins include STAT1, STAT3, STAT5, and STAT6, each of which has distinct functions in cellular responses:
- STAT1: Primarily involved in immune response regulation and defense against viral infections. It is activated by interferons and plays a key role in the antiviral immune response.
- STAT3: A critical player in inflammation, immune response, and cancer. STAT3 is frequently activated in tumors and is associated with promoting cell survival and proliferation.
- STAT5: Involved in regulating hematopoiesis and immune cell differentiation. It is activated by cytokines like interleukin-2 (IL-2) and is essential for T-cell development and function.
- STAT6: Activates genes involved in immune regulation, especially those responding to interleukin-4 (IL-4) and interleukin-13 (IL-13). STAT6 plays a significant role in allergic reactions and Th2 immune responses.
Once activated by phosphorylation by JAKs, STAT proteins dimerize (pair with another STAT protein) and translocate to the nucleus, where they act as transcription factors to regulate gene expression.
Cytokine Receptors: How Cytokine Receptors Initiate JAK STAT Signaling
The activation of the JAK/STAT pathway begins with the binding of cytokines to their corresponding cytokine receptors located on the surface of the target cell.
Cytokines are small signaling molecules that mediate communication between cells, especially in the immune system. Each cytokine receptor is associated with specific JAK proteins, which initiate the signaling process.
When a cytokine binds to its receptor, it induces a conformational change in the receptor, leading to the activation of the associated JAK proteins. These JAKs phosphorylate specific tyrosine residues on the receptor itself, creating docking sites for STAT proteins.
Once STATs bind to these phosphorylated sites, they are phosphorylated by JAKs, leading to their activation. Activated STAT proteins then form dimers, enter the nucleus, and initiate the transcription of target genes involved in immune responses, inflammation, and cell growth.
JAK/STAT Pathway in Health and Disease
The JAK/STAT pathway plays a pivotal role in maintaining cellular homeostasis and regulating numerous physiological processes, particularly in the immune system. However, when this pathway becomes dysregulated, it can contribute to the development of several diseases, including autoimmune disorders, inflammatory conditions, and various types of cancer.
Below, we explore the critical functions of the JAK/STAT pathway in health and its involvement in disease.
Role of the JAK STAT Pathway in the Immune Response
The JAK STAT pathway is essential for the immune system’s ability to respond to pathogens, regulate inflammation, and maintain immune tolerance. This pathway mediates the effects of cytokines, which are crucial signaling molecules in immune responses.
- Cytokine signaling: The JAK-STAT pathway transmits signals from a variety of cytokine receptors to initiate immune responses. For example, when interferons bind to their receptors, JAKs are activated, leading to the phosphorylation of STAT proteins, such as STAT1, which is critical for antiviral immunity.
- Immune cell activation and differentiation: The pathway also regulates the differentiation and activation of key immune cells, including T-cells, B-cells, and macrophages, which are central to adaptive immunity. STAT5, for instance, plays a significant role in T-cell development and function.
- Inflammation and immune response: By controlling the production of inflammatory cytokines and modulating immune cell behavior, the JAK-STAT pathway helps coordinate both acute and chronic immune responses.
Overall, the JAK-STAT pathway’s ability to regulate immune cell activation, differentiation, and the production of inflammatory mediators makes it a central component of the immune response.
The Involvement of the JAK/STAT Pathway in Inflammatory Diseases
Dysregulation of the JAK/STAT pathway is implicated in a variety of inflammatory diseases where immune responses are abnormally heightened or misdirected. In particular, overactive or uncontrolled JAK/STAT signaling contributes to chronic inflammation, tissue damage, and autoimmune responses.
- Rheumatoid Arthritis (RA): RA is a classic example of an inflammatory disease driven by aberrant JAK/STAT signaling. In RA, cytokines such as IL-6 and TNF-α activate the JAK/STAT pathway, leading to the production of additional inflammatory cytokines and chemokines. This chronic inflammation causes joint damage and pain. JAK inhibitors like Tofacitinib have been developed to block this pathway and offer therapeutic benefits by reducing inflammation and disease activity in RA patients.
- Other autoimmune disorders: Diseases such as psoriasis, Crohn’s disease, and systemic lupus erythematosus (SLE) also involve the dysregulation of the JAK-STAT pathway. In these conditions, the continuous activation of the pathway leads to excessive production of pro-inflammatory cytokines, contributing to tissue damage and chronic inflammation.
Therapies targeting JAK-STAT signaling are increasingly being used to treat these diseases by dampening the inappropriate immune responses and controlling inflammation.
JAK-STAT Signaling in Cancer: Implications in Leukemia, Lymphoma, and Solid Tumors
In addition to its role in immune regulation, the JAK-STAT pathway is heavily involved in the development and progression of several types of cancer, particularly hematological malignancies like leukemia and lymphoma, as well as solid tumors.
- Leukemia and Lymphoma: The JAK-STAT pathway is frequently activated in cancers of the blood, such as acute myeloid leukemia (AML), chronic myelogenous leukemia (CML), and non-Hodgkin lymphoma. In these cancers, mutations in JAK genes (such as JAK2 V617F) or the overproduction of certain cytokines lead to uncontrolled cell proliferation, survival, and resistance to apoptosis.
- Solid Tumors: JAK-STAT signaling also plays a role in the progression of solid tumors, including breast cancer, lung cancer, and colon cancer. STAT3, in particular, is frequently overactive in these cancers, promoting tumor cell survival, immune evasion, and metastasis. Targeting the JAK-STAT pathway in solid tumors is an area of active research, as inhibiting this signaling could potentially slow tumor growth and improve response to other therapies.
Targeting the JAK-STAT Pathway in Cancer Therapy
The JAK-STAT pathway’s involvement in cancer progression has made it an attractive target for cancer therapies. Aberrant activation of this pathway can drive tumor growth, immune evasion, and metastasis in various types of cancer.
Below, we explore the role of JAK inhibitors, the mechanisms by which the JAK-STAT pathway is modulated in cancer, and the promise and challenges of targeting this pathway in oncology.
JAK Inhibitors: Overview and Therapeutic Potential
JAK inhibitors are a class of targeted therapies designed to block the JAK-STAT signaling pathway, preventing the uncontrolled signaling that often drives cancer progression. These inhibitors have gained traction in the treatment of several hematologic and solid cancers due to their ability to interrupt key molecular signaling pathways involved in cell growth and survival.
- Tofacitinib: Originally developed for the treatment of autoimmune diseases like rheumatoid arthritis, Tofacitinib is an oral JAK inhibitor that targets JAK1 and JAK3. It has shown promise in treating myelofibrosis (a type of bone marrow cancer) and polycythemia vera (a blood cancer), by reducing the overactivation of JAK2, which is commonly implicated in these conditions.
- Ruxolitinib: This drug selectively inhibits JAK1 and JAK2 and has been approved for the treatment of myelofibrosis and polycythemia vera. By targeting the hyperactive JAK2 mutation (JAK2 V617F), Ruxolitinib helps reduce inflammation, control spleen size, and improve overall survival rates in patients with these hematologic malignancies. It has also shown potential in combination therapies for solid tumors.
These JAK inhibitors, along with others like Baricitinib and Fedratinib, are being explored in clinical trials to treat a range of cancers, particularly those where JAK-STAT signaling is known to be dysregulated.
Mechanisms of JAK STAT Pathway Modulation in Cancer
The JAK STAT pathway is frequently dysregulated in cancer, either through mutations in JAK proteins themselves or through overexpression of cytokines that activate the pathway. The modulation of this pathway in cancer primarily affects several key aspects of tumor biology:
- Tumor cell proliferation and survival: In many cancers, JAK STAT activation promotes tumor cell survival and proliferation. For example, STAT3 is often constitutively active in tumors, leading to the upregulation of genes involved in cell survival, angiogenesis, and immune suppression. Inhibiting JAKs or STATs can help induce apoptosis (cell death) and prevent the proliferation of tumor cells.
- Immune evasion: The JAK-STAT pathway is also involved in immune evasion by suppressing the immune system’s ability to detect and eliminate tumor cells. In tumors, this pathway can be hijacked to enhance the production of immunosuppressive cytokines like IL-10 and TGF-β, which inhibit the function of immune cells. By inhibiting JAK-STAT signaling, it is possible to restore immune function and improve anti-tumor immunity.
- Metastasis and angiogenesis: The pathway contributes to cancer metastasis (the spread of cancer cells to other parts of the body) by promoting the expression of genes involved in cell motility and invasion. It also promotes the formation of new blood vessels (angiogenesis), which tumors need to grow and spread. Targeting JAK-STAT signaling can hinder these processes and slow down tumor progression.
The Promise and Challenges of JAK-STAT-Based Therapies in Oncology
The potential of JAK-STAT-based therapies in cancer treatment is significant, as they offer a way to directly target the molecular mechanisms that drive tumor growth and progression. However, there are several challenges that must be addressed to maximize their clinical effectiveness:
Effectiveness in solid tumors:
While JAK inhibitors have shown clinical success in hematologic cancers like leukemia and myelofibrosis, their effectiveness in solid tumors has been more variable. The complex tumor microenvironment, including immune cells, stromal cells, and cytokine networks, can influence how these therapies perform.
More research is needed to determine how to best integrate JAK inhibitors with other treatments, such as chemotherapy, radiation, and immunotherapy, for solid tumors.
Resistance to therapy:
As with many targeted therapies, resistance to JAK inhibitors can develop over time. Cancer cells may adapt by upregulating alternative signaling pathways or by acquiring mutations that bypass the need for JAK-STAT signaling. Developing combination therapies that target multiple pathways or the use of second-generation JAK inhibitors is an active area of research to overcome this challenge.
Targeting specific STAT proteins:
While targeting JAKs is effective in some cases, selectively inhibiting specific STAT proteins, such as STAT3, could provide a more targeted therapeutic approach. Research is ongoing into developing small molecules or biologics that specifically inhibit STAT3 or other STAT proteins involved in cancer.
Conclusion
The JAK-STAT pathway plays a critical role in regulating cellular processes such as immune response, inflammation, and cell growth. Understanding the intricacies of JAK and STAT proteins, their activation, and signaling mechanisms is essential for unraveling their involvement in various diseases, including cancer and autoimmune disorders.
Targeting the JAK-STAT pathway with specific inhibitors holds promise for therapeutic interventions, especially in cancer treatment. Ongoing research continues to uncover new opportunities for modulating this pathway, potentially leading to more effective and targeted therapies in the future.