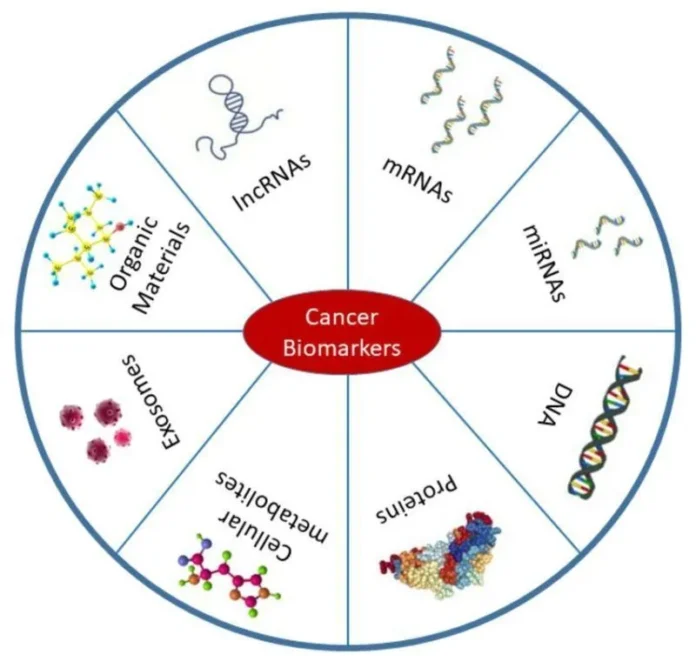
Cancer biomarkers are molecular substances that can be detected in tissues, blood, or other body fluids and serve as indicators of cancer presence, progression, or response to treatment.
These biomarkers provide crucial information about the tumor’s characteristics, helping healthcare professionals in the diagnosis, prognosis, and management of cancer.
They play an essential role in early detection, enabling treatment at a time when it is most likely to be successful.
Additionally, biomarkers are used to assess how a cancer may progress and predict how well a patient will respond to certain therapies.
In this blog post, we will explore the various types of cancer biomarkers and their significant impact on modern cancer care, focusing on how they contribute to more accurate diagnoses and personalized treatment plans.
Types of Cancer Biomarkers
Cancer biomarkers can be categorized into three main types: diagnostic, prognostic, and predictive. Each type plays a crucial role in different aspects of cancer care, from early detection to treatment planning.
Diagnostic Biomarkers
Diagnostic biomarkers are used to detect cancer at an early stage or even before symptoms appear. These biomarkers can be found in tissues or body fluids and provide a signal of the presence of cancer. For example, PSA (prostate-specific antigen) is a well-known biomarker for prostate cancer, and elevated levels are often associated with the disease.
Similarly, CA-125 is used for ovarian cancer detection, particularly in monitoring treatment response or detecting recurrence. Early detection biomarkers are vital for catching cancers such as breast, lung, and colorectal cancers, often leading to better treatment outcomes when detected early.
Prognostic Biomarkers
Prognostic biomarkers provide insights into the likely course of the disease, helping to predict cancer progression and patient survival. These biomarkers give clinicians a sense of how aggressive a cancer may be and how it might behave over time.
TP53 mutations, for example, are associated with a poorer prognosis in many cancers, including breast, lung, and colorectal cancers. Patients with these mutations often face a higher risk of recurrence or metastasis. Prognostic biomarkers help doctors determine the need for more intensive treatments and assist in long-term monitoring.
Predictive Biomarkers
Predictive biomarkers are used to identify which patients are likely to respond to specific cancer therapies. These biomarkers guide treatment decisions, allowing for more personalized care.
For instance, HER2 (human epidermal growth factor receptor 2) is a critical biomarker in breast cancer, and patients with HER2-positive tumors are often treated with targeted therapies like trastuzumab (Herceptin).
Similarly, EGFR (epidermal growth factor receptor) mutations are commonly found in non-small cell lung cancer and help identify patients who may benefit from EGFR-targeted therapies such as erlotinib.
Predictive biomarkers are essential for optimizing treatment regimens and minimizing unnecessary side effects by ensuring that therapies are tailored to individual patients.
Each type of biomarker plays an integral role in cancer management, helping to enhance early detection, predict outcomes, and guide therapy choices for more personalized, effective treatment strategies.
List of Cancer Biomarkers
Here’s an exhaustive list of biomarkers commonly used in cancer diagnosis, prognosis, and treatment prediction. These biomarkers span various cancer types, and their roles in cancer care are increasingly critical for precision medicine.
Diagnostic Biomarkers
- PSA (Prostate-Specific Antigen) – Prostate cancer
- CA-125 (Cancer Antigen 125) – Ovarian cancer
- HE4 (Human Epididymis Protein 4) – Ovarian cancer
- AFP (Alpha-Fetoprotein) – Liver cancer, germ cell tumors
- CA 19-9 – Pancreatic cancer, colorectal cancer
- CEA (Carcinoembryonic Antigen) – Colorectal cancer, breast cancer, lung cancer, pancreatic cancer
- HER2 (Human Epidermal Growth Factor Receptor 2) – Breast cancer, gastric cancer
- BRCA1/BRCA2 – Breast cancer, ovarian cancer
- EGFR (Epidermal Growth Factor Receptor) – Non-small cell lung cancer (NSCLC)
- ALK (Anaplastic Lymphoma Kinase) – Non-small cell lung cancer (NSCLC)
- VEGF (Vascular Endothelial Growth Factor) – Various cancers (angiogenesis marker)
- TP53 – Mutations in several cancers, including breast, colorectal, and ovarian cancer
- BCR-ABL – Chronic myelogenous leukemia (CML)
- PML-RARα – Acute promyelocytic leukemia (APL)
- MMPs (Matrix Metalloproteinases) – Various cancers (involved in metastasis)
- c-Met (Hepatocyte Growth Factor Receptor) – Gastric cancer, lung cancer, and others
- SCCA (Squamous Cell Carcinoma Antigen) – Squamous cell carcinoma (lung, cervical cancer)
Prognostic Biomarkers
- TP53 mutations – Poor prognosis in several cancers (e.g., breast, lung, colorectal)
- KRAS mutations – Colorectal cancer, pancreatic cancer, lung cancer
- P16 (INK4a) – Cervical cancer, head and neck cancers (poor prognosis in HPV-negative cancers)
- PI3K/AKT pathway mutations – Various cancers (e.g., breast, ovarian, and colorectal)
- BCL-2 (B-cell lymphoma 2) – Lymphoma, chronic lymphocytic leukemia (CLL), breast cancer
- Ki-67 – Proliferation marker, various cancers (e.g., breast, prostate)
- MCM (Minichromosome Maintenance Proteins) – Cancer progression marker
- Vimentin – Marker for epithelial-to-mesenchymal transition (EMT) in various cancers
- EGFR mutations – Non-small cell lung cancer (NSCLC)
- TGF-β (Transforming Growth Factor Beta) – Metastasis and poor prognosis in several cancers
Predictive Biomarkers
- HER2 (Human Epidermal Growth Factor Receptor 2) – Breast cancer, gastric cancer (predicts response to trastuzumab)
- EGFR mutations – Non-small cell lung cancer (predicts response to EGFR inhibitors)
- ALK rearrangements – Non-small cell lung cancer (predicts response to ALK inhibitors)
- KRAS mutations – Colon cancer (predicts response to EGFR inhibitors)
- PD-L1 (Programmed Death-Ligand 1) – Various cancers (predicts response to immune checkpoint inhibitors)
- BRCA1/BRCA2 mutations – Breast cancer, ovarian cancer (predicts response to PARP inhibitors)
- MSI (Microsatellite Instability) – Colorectal cancer, endometrial cancer (predicts response to immunotherapy)
- MLH1, MSH2, MSH6, PMS2 – DNA mismatch repair genes (predict response to immunotherapy in Lynch syndrome-related cancers)
- BRAF mutations – Melanoma, colorectal cancer (predicts response to BRAF inhibitors)
- PD-1 (Programmed Cell Death Protein 1) – Various cancers (predicts response to immune checkpoint inhibitors)
- TMB (Tumor Mutational Burden) – Various cancers (predicts response to immunotherapy)
- C-Met – Gastric cancer, lung cancer (predicts response to MET inhibitors)
- PIK3CA mutations – Breast cancer (predicts response to PI3K inhibitors)
- VEGF – Various cancers (predicts response to anti-angiogenic therapies)
- AR (Androgen Receptor) – Prostate cancer (predicts response to androgen deprivation therapy)
Cancer-Specific Biomarkers
- CA 15-3 – Breast cancer (used for monitoring treatment and recurrence)
- CA 27.29 – Breast cancer (monitoring biomarker)
- Chromogranin A – Neuroendocrine tumors
- S100B – Melanoma (used for monitoring therapy and metastasis)
- Thyroglobulin – Thyroid cancer
- AFP-L3 (Alpha-fetoprotein) – Hepatocellular carcinoma
- M2-PK (Pyruvate Kinase Isoenzyme M2) – Colorectal cancer
- MALAT1 (Metastasis-associated lung adenocarcinoma transcript 1) – Lung cancer
- Gastrin – Gastric cancer
- NSE (Neuron-Specific Enolase) – Small cell lung cancer, neuroblastoma
Emerging and Experimental Biomarkers
- Circulating Tumor DNA (ctDNA) – Various cancers (used in liquid biopsy for monitoring treatment and detecting recurrence)
- Circulating Tumor Cells (CTCs) – Various cancers (early detection and monitoring metastasis)
- Exosomal RNA – Various cancers (used in liquid biopsy for detection and monitoring)
- MicroRNAs (miRNAs) – Various cancers (used for diagnosis, prognosis, and predicting therapy responses)
- Long Non-Coding RNAs (lncRNAs) – Various cancers (emerging biomarkers for cancer detection and prognosis)
- Tissue-specific miRNAs – Various cancers (early detection, therapy response)
This list includes biomarkers across different categories—diagnostic, prognostic, predictive, and emerging biomarkers—involved in cancer care.
Methods of Identifying and Testing Cancer Biomarkers
Traditional Tissue Biopsy
Traditional tissue biopsy is a commonly used method for diagnosing and identifying cancer biomarkers. In this process, a sample of tissue is collected from the tumor through a surgical procedure or a needle biopsy.
This sample is then examined in a laboratory for the presence of specific biomarkers that can provide crucial insights into the cancer’s characteristics and behavior.
Pros:
- Direct Analysis: Tissue biopsy provides a direct sample from the tumor, ensuring that the biomarkers analyzed are representative of the cancer’s biological features.
- Accurate Diagnosis: It allows for the identification of genetic mutations (e.g., KRAS mutations in colorectal cancer), protein expressions (e.g., HER2 in breast cancer), and other molecular alterations that help guide treatment decisions.
- Histopathological Examination: It enables the assessment of tumor grade, staging, and other critical factors that influence treatment planning.
Cons:
- Invasive: Tissue biopsy is an invasive procedure, often requiring local or general anesthesia. This can cause discomfort and potential complications such as infection or bleeding.
- Limited Sample Size: A single biopsy may not capture the full heterogeneity of a tumor, meaning it may not reflect all the genetic mutations or other biomarkers present in the tumor.
- Risk of Complications: As with any surgical procedure, tissue biopsy carries a risk of complications, such as pain, bleeding, or infection at the biopsy site.
Common biomarkers tested in tissue biopsies include KRAS mutations (for colorectal cancer), TP53 mutations, EGFR mutations (for lung cancer), and HER2 overexpression (for breast cancer). These biomarkers are crucial in making decisions about the most effective treatments and therapies for individual patients.
Liquid Biopsy
Liquid biopsy is a non-invasive, emerging method for detecting cancer biomarkers. Instead of requiring a tissue sample, liquid biopsy analyzes biological fluids, such as blood, urine, or saliva, to detect biomarkers associated with cancer.
This method is becoming increasingly popular due to its convenience and potential to detect cancer earlier, monitor progression, and track treatment response in real-time.
Definition and Advantages Over Traditional Biopsy:
- Non-Invasive: Liquid biopsy requires only a blood draw or other fluid samples, eliminating the need for invasive tissue sampling, which reduces patient discomfort and complications.
- Real-Time Monitoring: It allows for continuous monitoring of tumor dynamics, enabling clinicians to assess how the tumor is responding to treatment without the need for repeated biopsies.
- Detection of Early-Stage Cancer: Liquid biopsy can detect cancer at an early stage, even before the tumor is large enough to be visible on imaging scans. This is especially valuable in cancers that are difficult to detect early, such as ovarian or pancreatic cancer.
Biomarkers Detected in Blood:
- ctDNA (Circulating Tumor DNA): ctDNA is fragments of DNA shed by tumors into the bloodstream. It contains genetic mutations and alterations found in the tumor, making it a powerful tool for detecting and monitoring cancer. ctDNA can be used to identify mutations such as KRAS or EGFR, and monitor treatment response.
- Circulating Tumor Cells (CTCs): CTCs are cancer cells that have broken away from the primary tumor and entered the bloodstream. The presence of CTCs can indicate the spread of cancer (metastasis) and help track the progression of the disease.
- Exosomal RNA and miRNAs: Exosomes are small vesicles secreted by cancer cells that carry RNA and proteins. Analyzing the RNA content in exosomes can provide valuable information about the tumor’s genetic makeup and how it might respond to therapies.
Applications in Early Cancer Detection and Monitoring Therapy Response:
- Early Detection: Liquid biopsy is increasingly being used for early cancer detection, offering a less invasive and potentially more accessible way to identify cancer biomarkers at an earlier stage than traditional methods.
- Monitoring Treatment Response: Liquid biopsy is a valuable tool for assessing how well a patient’s cancer is responding to treatment. By tracking the levels of ctDNA or CTCs, clinicians can determine whether the tumor is shrinking, stable, or developing resistance to therapy.
- Minimal Residual Disease Detection: Liquid biopsy can detect minimal residual disease (MRD)—small amounts of cancer cells left after treatment that may cause relapse. This is especially helpful in monitoring cancers like leukemia and lymphoma.
Emerging Technologies and Advancements in Biomarker Discovery
Proteomic Biomarkers
Proteomic biomarkers are proteins found in tissues, blood, and other bodily fluids that can provide valuable information about cancer. These biomarkers are particularly useful in detecting cancer, assessing tumor characteristics, and guiding treatment decisions.
Use of Protein Biomarkers for Cancer Detection
Proteins play critical roles in the development and progression of cancer. One well-known example is HER2 (human epidermal growth factor receptor 2), a protein that is overexpressed in some breast cancers.
Testing for HER2 expression helps determine whether patients are candidates for targeted therapies like trastuzumab (Herceptin). Other protein biomarkers, such as CA-125 in ovarian cancer or PSA in prostate cancer, are widely used for monitoring and diagnosing cancer.
Proteomic Profiling in Personalized Cancer Therapy
Proteomic profiling involves analyzing the proteins expressed by a tumor to understand its molecular makeup. This approach can identify specific proteins or changes in protein expression that are associated with cancer subtypes.
By profiling a patient’s tumor, clinicians can tailor treatment strategies to target specific proteins or signaling pathways that drive cancer growth. For instance, targeting EGFR in non-small cell lung cancer or BRAF mutations in melanoma has shown clinical success. Proteomic biomarkers are becoming increasingly important in precision medicine, allowing for more individualized and effective treatment options.
Gene Expression Biomarkers
Gene expression biomarkers reflect the activity of genes in the tumor and surrounding tissue. By analyzing the expression levels of certain genes, clinicians can gain insights into cancer’s behavior, predict prognosis, and assess potential therapeutic responses.
Role of Gene Expression in Cancer Diagnosis and Treatment: Genes like BRCA1 and BRCA2 are essential for maintaining the stability of the genome, and mutations in these genes are linked to an increased risk of breast and ovarian cancers.
Testing for mutations in these genes helps guide treatment decisions, such as the use of PARP inhibitors for patients with BRCA mutations. Gene expression profiling can also identify cancer subtypes with distinct behaviors, which is crucial for selecting the most appropriate treatment.
How Genetic Signatures Can Predict Patient Outcomes: In addition to individual biomarkers, genetic signatures—patterns of gene expression across multiple genes—can be used to predict cancer prognosis and treatment response.
For example, a genetic signature of estrogen receptor-positive (ER+) breast cancer can help predict how well a patient will respond to hormone therapy. Similarly, in lung cancer, gene expression profiling can help identify patients likely to benefit from targeted therapies.
These genetic signatures enable more accurate predictions of patient outcomes, leading to personalized treatment plans that optimize survival and minimize unnecessary side effects.
Conclusion
Cancer biomarkers play a pivotal role in the diagnosis, prognosis, and treatment of cancer. From traditional tissue biopsies to advanced methods like liquid biopsy and next-generation sequencing, the continuous evolution of biomarker discovery holds immense potential for personalized cancer therapy.