Cancer immunotherapy represents a revolutionary approach to treating cancer, leveraging the body’s own immune system to recognize and eradicate malignant cells. This groundbreaking field represents a paradigm shift in the approach to cancer treatment.
What is cancer immunotherapy?
Cancer immunotherapy is a specialized form of cancer treatment that utilizes the body’s immune system to recognize, target, and eliminate cancer cells. The immune system, which is naturally designed to identify and destroy abnormal or foreign cells, can sometimes fail to recognize cancer cells as a threat. Cancer immunotherapies aim to overcome this evasion by enhancing the immune system’s ability to detect and attack cancer.
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful invaders, including bacteria, viruses, and abnormal cells like cancer cells. However, cancer cells can sometimes evade detection by the immune system or create an immunosuppressive environment, allowing them to grow and spread.
Research in cancer immunotherapy is ongoing, with scientists exploring new strategies, combination approaches, and personalized treatments to further enhance its efficacy and broaden its application to different types of cancer.
How successful is immunotherapy for cancer?
The success of immunotherapy for cancer varies depending on the type of cancer, the stage at which it is diagnosed, and individual patient factors. Immunotherapy has shown remarkable success in certain cancers, leading to durable responses and improved outcomes in some patients. However, it’s essential to understand that not all patients respond to immunotherapy, and the level of success can vary. Overall response rates are about 15 to 20%.
Successes and Breakthroughs
Cancer immunotherapy has demonstrated remarkable success in the treatment of various cancers. Drugs like pembrolizumab and nivolumab, both PD-1 inhibitors, have shown significant efficacy against melanoma, lung cancer, and other malignancies.
CAR-T cell therapy has achieved remarkable responses in certain types of leukemia and lymphoma, leading to durable remissions in some patients. These breakthroughs have provided new hope for individuals facing previously untreatable cancers.
What type of cancers does immunotherapy cure?
Immunotherapy has shown significant success in treating certain types of cancer, leading to durable responses and improved outcomes in some patients. However, the effectiveness of immunotherapy can vary depending on the type of cancer and individual patient factors. Here is a list of cancers treated with immunotherapy drugs:
- Melanoma: Immunotherapy, particularly PD-1 inhibitors like pembrolizumab and nivolumab, has shown significant success in treating advanced melanoma.
- Lung Cancer: Non-small cell lung cancer (NSCLC) has been treated with PD-1 and PD-L1 inhibitors, either as monotherapy or in combination with chemotherapy.
- Hodgkin’s Lymphoma: PD-1 inhibitors have demonstrated effectiveness in treating Hodgkin’s lymphoma, especially in cases where other treatments have failed.
- Renal Cell Carcinoma: Advanced renal cell carcinoma has responded well to immune checkpoint inhibitors targeting PD-1 and CTLA-4.
- Bladder Cancer: PD-1 and PD-L1 inhibitors have been approved for the treatment of advanced bladder cancer, offering a new therapeutic option.
- Head and Neck Cancer: Immunotherapy, including PD-1 inhibitors, has been used to treat certain types of head and neck cancers, particularly in cases that have not responded well to other treatments.
- Colorectal Cancer: Some patients with microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR) colorectal cancer may benefit from immunotherapy.
- Liver Cancer: Immunotherapy has been investigated as a treatment for hepatocellular carcinoma (HCC), the most common type of liver cancer.
- Gastric Cancer: PD-1 inhibitors have been explored as a treatment option for advanced gastric or gastroesophageal junction cancer.
- Breast Cancer: Some ongoing clinical trials are evaluating the effectiveness of immunotherapy, particularly PD-1/PD-L1 inhibitors, in certain subtypes of breast cancer.
- Ovarian Cancer: There are three FDA-approved immunotherapy treatments for ovarian cancer including targeted antibodies and immunomodulators.
- Pancreatic Cancer: There is two FDA-approved immunotherapy ( Dostarlimab and Pembrolizumab ) for a small subset of patients with pancreatic cancer, and many more are in clinical trials.
- Prostate Cancer: Some patients with microsatellite instability-high (MSI-H) and mismatch repair-deficient (dMMR) may benefit from immunotherapy.
- Leukemia: There are currently ten FDA-approved immunotherapy options for leukemia including targeted antibodies, adoptive cell therapy, and immunomodulators.
- Brain Cancer: There are currently six FDA-approved immunotherapy treatments for brain cancer including immunomodulators and targeted antibodies.
Types of cancer immunotherapy
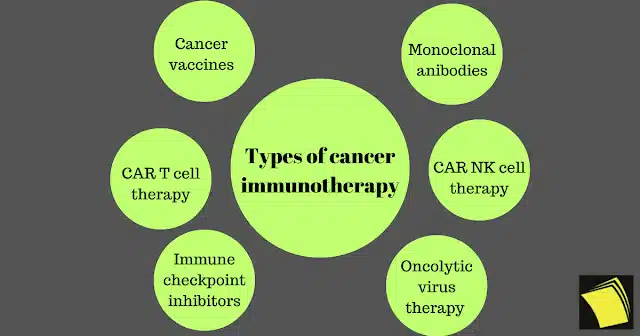
There are several types of cancer immunotherapy, each designed to harness the body’s immune system to target and destroy cancer cells. Here are some key types of cancer immunotherapy:
- Monoclonal antibodies (MABs)
- Checkpoint Inhibitors
- Cancer vaccines
- CAR T-cell therapy
- CAR NK cell therapy
- Oncolytic virus therapy
- Cytokines
Cytokines
Cytokines: Interleukins and interferons are types of proteins known as cytokines that can be administered to stimulate the immune system. Interleukin-2 (IL-2) and interferon-alpha are examples used in cancer immunotherapy.
Checkpoint inhibitors
These drugs block specific proteins on immune cells or cancer cells, preventing them from inhibiting the immune response. Examples include PD-1 inhibitors (pembrolizumab, nivolumab) and CTLA-4 inhibitors (ipilimumab).
Monoclonal antibodies
These are laboratory-produced molecules that can mimic the immune system’s ability to fight off harmful pathogens, including cancer cells. Monoclonal antibodies can be designed to target specific proteins on cancer cells. Examples include trastuzumab (Herceptin) for HER2-positive breast cancer and rituximab (Rituxan) for certain types of lymphoma.
CAR T cell therapy
T cells, integral components of the immune system, combat infections. In the context of T-cell therapy, physicians extract T cells from the bloodstream. Subsequently, a laboratory introduces specific receptors to these cells.
These receptors enable the modified T cells to identify and target cancer cells. The modified T cells are then reintroduced into the patient’s body, where they locate and eliminate cancerous cells. This therapeutic approach is referred to as chimeric antigen receptor (CAR) T-cell therapy.
CAR T-cell therapy is applied in the treatment of specific blood cancers. Ongoing research continues to explore this therapy and alternative methods for modifying T cells to effectively address cancer.
CAR NK cell therapy
CAR NK cell therapy, or Chimeric Antigen Receptor Natural Killer cell therapy, is an innovative form of cancer immunotherapy. Natural Killer (NK) cells are a type of immune cell with the inherent ability to recognize and destroy abnormal cells, including cancer cells. In CAR NK cell therapy, these cells are genetically engineered to express Chimeric Antigen Receptors (CARs) on their surface.
Cancer vaccines
A cancer vaccine plays a crucial role in enhancing your body’s ability to combat diseases. By exposing your immune system to a foreign protein, known as an antigen, a vaccine stimulates the immune system to recognize and eliminate the antigen or related substances. Cancer vaccines come in two main types: prevention vaccines and treatment vaccines.
An illustration of a cancer prevention vaccine is Gardasil, designed to safeguard against the human papillomavirus (HPV), a virus linked to specific cancer types. Conversely, a treatment vaccine like spuleucel-T (Provenge) targets advanced prostate cancer unresponsive to hormone therapy.
Oncolytic virus therapy
Oncolytic virus therapy, sometimes referred to simply as virus therapy, employs laboratory-altered viruses to eliminate cancer cells. A genetically modified variant of the virus is introduced into the tumor, where it reproduces upon entering cancer cells.
This replication process leads to the bursting and demise of cancer cells. As these cells perish, they release proteins that stimulate the immune system to target other cancer cells throughout the body displaying similar proteins, effectively amplifying the immune response. Importantly, the virus is engineered to avoid entering healthy cells.
Currently, the United States has approved one form of oncolytic virus therapy for cancer treatment: Talimogene laherparepvec (Imlygic) or T-VEC.
This therapy is sanctioned for advanced melanoma cases that are not amenable to surgical intervention, particularly for individuals who cannot or choose not to pursue alternative recommended treatments. T-VEC, derived from the herpes simplex virus responsible for cold sores, is directly injected into one or more melanoma tumors.
Ongoing clinical trials are exploring the effectiveness of various oncolytic viruses for diverse cancers. Additionally, these trials investigate the synergy between oncolytic viruses and other cancer treatments, such as chemotherapy.
How is immunotherapy done?
Immunotherapy can be administered in various ways, and the specific method depends on the type of immunotherapy and the type of cancer being treated. Here are some common methods of immunotherapy administration:
- Intravenous (IV) Infusion: Many immunotherapy drugs are administered directly into the bloodstream through a vein. This is typically done in a clinic or hospital setting. The infusion process may take several hours, and patients are monitored during and after the infusion for any potential reactions.
- Subcutaneous (SC) Injection: Some immunotherapy drugs can be injected under the skin. This method is often used for certain types of immunotherapy, such as checkpoint inhibitors. Patients may receive these injections in a clinic, and the frequency can vary depending on the treatment plan.
- Oral Medications: Some immunotherapy drugs are available in pill or capsule form, and patients can take them orally at home. This method is more convenient for some patients and allows for greater flexibility in the treatment schedule.
- Intravesical Administration: In cases of bladder cancer, immunotherapy may be administered directly into the bladder through a catheter. This method allows the treatment to target cancer cells in the bladder while minimizing exposure to the rest of the body.
- Intradermal Injection: In certain situations, immunotherapy may be administered as an injection just under the skin. This method is less common but may be used for specific types of treatments.
- Intratumoral Injection: In some cases, immunotherapy may be injected directly into a tumor. This method aims to stimulate the immune response within the tumor itself.
Immunotherapy side effects
While immunotherapy can be effective, it may also cause various side effects. It’s important to note that not everyone experiences these side effects, and their severity can vary. Common immunotherapy side effects include:
- Fatigue: Feeling tired or weak is a common side effect. It’s essential to get enough rest and inform your healthcare team if fatigue becomes severe.
- Skin reactions: Skin problems such as rash, itching, or redness may occur. These reactions are often manageable with topical treatments.
- Flu-like symptoms: Fever, chills, muscle aches, and headache can occur shortly after receiving immunotherapy. These symptoms are usually temporary and can be treated with over-the-counter medications.
- Nausea and diarrhea: Some people may experience digestive issues, including nausea, diarrhea, or loss of appetite. Your healthcare team can provide medications to alleviate these symptoms.
- Breathing difficulties: Immunotherapy can cause inflammation in the lungs, leading to shortness of breath or cough. It’s crucial to report any respiratory symptoms to your healthcare provider.
- Hormone-related side effects: Certain immunotherapies can affect hormone levels, leading to conditions such as thyroid dysfunction. Regular monitoring and hormone replacement therapy may be necessary.
- Liver problems: Immunotherapy can impact liver function, resulting in elevated liver enzymes. Regular blood tests can monitor these changes, and your healthcare team will intervene if needed.
- Allergic reactions: In rare cases, individuals may experience severe allergic reactions (anaphylaxis) to immunotherapy. This can cause difficulty breathing, swelling, or a drop in blood pressure and requires immediate medical attention.
It’s crucial to communicate openly with your healthcare team about any side effects you experience. They can provide guidance on managing symptoms and may adjust your treatment plan if necessary. Furthermore, It’s also essential to attend scheduled follow-up appointments and undergo recommended monitoring to ensure early detection and management of any potential side effects.
Conclusion
As we stand at the frontier of this medical revolution, the promise of immunotherapy shines bright. It’s a testament to human ingenuity and the relentless pursuit of solutions to one of humanity’s greatest challenges. The journey into cancer immunotherapy is not just a scientific expedition; it’s a beacon of hope illuminating the path toward a future where cancer’s grip is loosened, and lives are transformed.