Adrenal carcinoma, also known as adrenocortical carcinoma, is a rare but aggressive cancer that originates in the adrenal glands—small, triangular-shaped organs located above the kidneys.
These glands play a vital role in hormone production, regulating essential body functions like metabolism, immune response, and blood pressure. While adrenal carcinoma is uncommon, its impact can be significant due to the disruption of hormonal balance and the potential for metastasis.
In this blog post, we’ll explore the causes, symptoms, diagnostic methods, and treatment options for adrenal carcinoma, offering insights into this complex condition and the latest advancements in its management.
What is Adrenal Carcinoma?
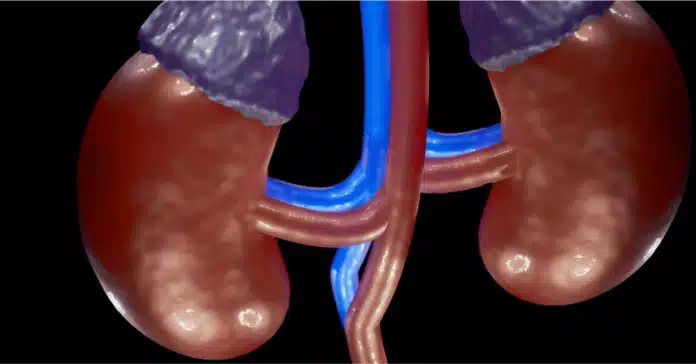
Overview of Adrenal Glands
The adrenal glands are two small, triangular-shaped organs located on top of each kidney. Despite their size, they play a crucial role in maintaining the body’s balance by producing essential hormones. These glands consist of two main parts:
- Adrenal Cortex: The outer layer, responsible for producing steroid hormones such as cortisol (regulates stress and metabolism), aldosterone (controls blood pressure and electrolyte balance), and androgens (sex hormones).
- Adrenal Medulla: The inner layer, which produces catecholamines like adrenaline and noradrenaline that help regulate the “fight or flight” response.
Understanding Adrenal Carcinoma
Adrenal carcinoma, also known as adrenocortical carcinoma (ACC), is a rare and aggressive cancer that originates in the adrenal cortex. Unlike benign adrenal tumors (such as adenomas), adrenal carcinoma is malignant and can spread to other parts of the body.
- Adrenal Adenoma vs. Adrenal Carcinoma: Adenomas are non-cancerous growths that rarely pose significant health risks and are often discovered incidentally. In contrast, adrenal carcinoma is life-threatening, often requiring immediate treatment due to its aggressive nature.
- Prevalence and Rarity: Adrenal carcinoma is exceedingly rare, with an estimated incidence of 1–2 cases per million people annually. It can occur at any age but is more commonly diagnosed in children under 5 and adults in their 40s and 50s.
Types of Adrenal Tumors
Adrenal tumors can be classified based on their ability to produce hormones:
- Hormone-Secreting Tumors:
- These tumors produce excess hormones, leading to specific syndromes like Cushing’s syndrome (due to cortisol overproduction) or hyperaldosteronism (caused by excess aldosterone).
- Symptoms often include weight gain, high blood pressure, and changes in physical appearance.
- Non-Secreting Tumors:
- These tumors do not produce excess hormones but may still cause symptoms if they grow large enough to press against nearby organs.
- Comparison with Pheochromocytoma:
- While adrenal carcinoma arises in the adrenal cortex, pheochromocytomas are rare tumors that develop in the adrenal medulla. Unlike adrenal carcinoma, pheochromocytomas primarily overproduce catecholamines, causing symptoms like severe hypertension, palpitations, and headaches.
Causes and Risk Factors of Adrenal Carcinoma
Adrenal carcinoma, like many cancers, often develops due to a combination of genetic, environmental, and biological factors. While the exact cause remains unknown in most cases, researchers have identified several risk factors and underlying mechanisms that may contribute to its development.
Genetic and Hereditary Factors
- Li-Fraumeni Syndrome: This rare genetic disorder, caused by mutations in the TP53 tumor suppressor gene, is strongly associated with an increased risk of adrenal carcinoma, particularly in children.
- Beckwith-Wiedemann Syndrome: A genetic condition characterized by overgrowth and a higher predisposition to certain cancers, including adrenal carcinoma.
- Familial Adenomatous Polyposis (FAP): A hereditary condition involving mutations in the APC gene, which can occasionally lead to adrenal tumors.
Inherited genetic mutations impair the body’s ability to regulate cell growth and repair DNA damage, increasing the risk of developing malignant tumors in the adrenal glands.
Hormonal Imbalances and Conditions
Excess hormone production in the adrenal glands can sometimes contribute to tumor growth. Conditions such as Cushing’s syndrome (caused by excessive cortisol production) or hyperaldosteronism (linked to overproduction of aldosterone) may increase the risk of adrenal tumors, though the exact relationship is not fully understood.
Additionally, hormonal fluctuations during certain life stages, such as puberty or pregnancy, may contribute to tumor development, though more research is needed.
Age and Demographic Influences
- Age: Adrenal carcinoma has a bimodal age distribution, meaning it is more commonly diagnosed in young children under 5 years old and in adults between the ages of 40 and 50.
- Gender: Studies suggest that women are slightly more likely to develop adrenal carcinoma than men, although the reasons for this are unclear.
Environmental and Lifestyle Factors
While no direct environmental cause has been confirmed, potential contributing factors may include:
- Exposure to Carcinogens: Prolonged exposure to environmental toxins, such as industrial chemicals or pesticides, may increase the risk of developing adrenal carcinoma.
- Lifestyle Factors: Although evidence is limited, unhealthy habits like smoking and poor diet could indirectly contribute to cancer risk by increasing systemic inflammation and oxidative stress.
Idiopathic Cases
In many instances, adrenal carcinoma occurs without any identifiable risk factors. These cases are considered idiopathic, highlighting the need for continued research into the molecular mechanisms driving this rare cancer.
Signs, Symptoms, and Diagnosis
Adrenal carcinoma can present with a wide range of symptoms depending on whether the tumor is hormone-secreting or non-secreting. Early detection is challenging, as symptoms are often nonspecific or related to hormone overproduction. Proper diagnosis requires a combination of clinical evaluation, imaging, and laboratory tests.
Signs and Symptoms of Adrenal Carcinoma
- Hormone-Related Symptoms (in hormone-secreting tumors):
- Cushing’s Syndrome: Excess cortisol production can cause weight gain (especially in the face and abdomen), muscle weakness, high blood pressure, diabetes, and purple stretch marks.
- Hyperaldosteronism: Overproduction of aldosterone leads to high blood pressure, low potassium levels, muscle cramps, and excessive thirst or urination.
- Virilization (in women): Excess production of androgens can cause male-pattern hair growth, deepening of the voice, and irregular menstrual cycles.
- Feminization (in men): Excess estrogen production can result in gynecomastia (breast tissue growth) and reduced libido.
- General Symptoms (in both hormone-secreting and non-secreting tumors):
- Persistent abdominal pain or discomfort.
- A palpable mass in the abdomen or flank region.
- Unexplained weight loss.
- Fatigue or weakness.
- Symptoms Due to Tumor Growth:
- Large tumors can press against nearby organs, causing pain or difficulty with digestion.
Diagnostic Tests and Imaging
- Clinical Evaluation:
- A detailed medical history and physical examination to assess symptoms of hormonal imbalances or a palpable mass.
- Hormonal Blood and Urine Tests:
- Cortisol levels: To check for Cushing’s syndrome.
- Aldosterone and renin levels: To diagnose hyperaldosteronism.
- Androgens and estrogens: To identify excess hormone production.
- Imaging Studies:
- CT Scan: High-resolution imaging to identify tumor size, location, and spread to nearby organs.
- MRI: Useful for detailed imaging, particularly for soft tissue and vascular involvement.
- PET Scan: Helps detect metastasis and assess tumor activity.
- Biopsy of Adrenal Tumors:
- Although rarely performed due to the risk of tumor spread, a biopsy may be considered in specific cases to confirm malignancy.
Differential Diagnosis
Adrenal carcinoma shares symptoms with other adrenal conditions, making accurate diagnosis critical. Common conditions to differentiate include:
- Adrenal Adenoma: A benign tumor that may or may not produce hormones.
- Pheochromocytoma: A tumor of the adrenal medulla that causes excess production of catecholamines, leading to high blood pressure, palpitations, and headaches.
- Metastatic Tumors: Secondary cancers that spread to the adrenal glands from other primary sites like the lung or breast.
Staging and Prognosis
After diagnosis, adrenal carcinoma is staged based on tumor size, lymph node involvement, and metastasis (TNM staging system). Staging helps determine the prognosis and guide treatment decisions.
- Stage I–II: Tumors confined to the adrenal gland.
- Stage III–IV: Advanced tumors that invade nearby organs or metastasize to distant sites, such as the liver or lungs.
Early recognition of symptoms and a thorough diagnostic workup are critical for effective management and improving survival outcomes in adrenal carcinoma.
Treatment Options for Adrenal Carcinoma
The treatment of adrenal carcinoma depends on the tumor’s stage, size, and whether it has spread to other parts of the body. A multidisciplinary approach, often involving surgery, medication, and sometimes radiation or chemotherapy, is used to manage this aggressive cancer effectively.
1. Surgery: The Primary Treatment
- Adrenalectomy:
- The complete surgical removal of the affected adrenal gland is the gold standard for treating adrenal carcinoma.
- In early-stage tumors (Stage I–II), surgery offers the best chance for a cure.
- Laparoscopic adrenalectomy may be used for smaller tumors, but open surgery is preferred for larger or invasive tumors to ensure complete removal.
- Debulking Surgery:
- In cases of advanced cancer (Stage III–IV), debulking surgery may be performed to reduce tumor size and alleviate symptoms, even if complete removal isn’t possible.
2. Medications and Targeted Therapy
- Mitotane:
- A specialized drug used to target adrenal cancer cells and inhibit hormone production by the adrenal cortex.
- Often prescribed after surgery to reduce the risk of recurrence or in cases where surgery isn’t an option.
- Side effects may include nausea, fatigue, and neurological symptoms, requiring careful monitoring.
- Hormone Therapy:
- In hormone-secreting tumors, additional medications may be used to manage excess hormone production, such as ketoconazole or metyrapone.
- Targeted Therapy:
- While not yet standard, ongoing research explores therapies targeting specific genetic mutations or pathways involved in adrenal carcinoma.
3. Radiation Therapy
- External Beam Radiation:
- Used in cases where surgery isn’t feasible or to manage symptoms caused by metastatic tumors.
- Often combined with other treatments to improve local control of the tumor.
- Palliative Radiation:
- Helps relieve pain and discomfort caused by tumor growth or metastasis.
4. Chemotherapy
- Systemic Chemotherapy:
- Used for advanced or metastatic adrenal carcinoma, particularly when surgery and other treatments are ineffective.
- Commonly used drugs include etoposide, cisplatin, doxorubicin, and streptozocin.
- Chemotherapy is often combined with mitotane for better outcomes, although its efficacy in adrenal carcinoma is limited compared to other cancers.
5. Emerging and Experimental Treatments
- Immunotherapy:
- Promising research suggests immunotherapy may improve outcomes by stimulating the immune system to target cancer cells. Drugs like checkpoint inhibitors are under investigation for adrenal carcinoma.
- Clinical Trials:
- Patients with advanced or recurrent adrenal carcinoma may benefit from enrolling in clinical trials exploring innovative therapies, such as novel targeted drugs or combination treatments.
6. Multimodal Approach and Supportive Care
- Combination Therapy:
- Advanced cases often require a combination of surgery, medication, and radiation to manage the disease effectively.
- Palliative Care:
- Focuses on improving the quality of life for patients with advanced adrenal carcinoma, addressing symptoms such as pain, fatigue, or hormonal imbalances.
Factors Influencing Treatment Choice
- Tumor Stage: Early-stage tumors are often curable with surgery, while advanced-stage cancers may require systemic therapies.
- Patient Health: Age, overall health, and the ability to tolerate treatment play a significant role in determining the best approach.
- Hormonal Activity: Hormone-secreting tumors require additional management to control hormone-related symptoms.
Advancements in surgical techniques, targeted therapies, and supportive care are improving outcomes for adrenal carcinoma patients. However, early detection and a tailored treatment plan remain critical for achieving the best possible prognosis.
Conclusion
Adrenal carcinoma is a rare but aggressive cancer that requires early detection and a multidisciplinary treatment approach for optimal outcomes. Understanding its causes, symptoms, and treatment options empowers patients and healthcare providers to make informed decisions. While advancements in surgery, medications, and emerging therapies are improving outcomes, continued research is essential to uncover better diagnostic tools and targeted treatments. Raising awareness about this condition can lead to earlier diagnoses and better management, offering hope to those affected.
Frequently Asked Questions (FAQs)
What is the survival rate for adrenal carcinoma?
The survival rate for adrenal carcinoma depends on the stage at diagnosis and the effectiveness of treatment. For localized tumors (Stages I and II), the 5-year survival rate is approximately 50-60%, provided the cancer is completely removed through surgery. For advanced stages (Stages III and IV), the survival rate drops significantly to around 10-20%, especially if the cancer has spread to distant organs. Early detection and prompt treatment are crucial for improving survival outcomes.
What are the symptoms of adrenal cancer?
Symptoms of adrenal cancer vary depending on whether the tumor is hormone-secreting or non-secreting. Common signs include:
- Hormonal symptoms: Weight gain, muscle weakness, high blood pressure, excessive hair growth (virilization), or breast tissue growth in men (feminization).
- General symptoms: Persistent abdominal or flank pain, unexplained weight loss, and fatigue.
- Tumor-related symptoms: A palpable mass in the abdomen or signs of pressure on nearby organs.
Is adrenal cancer treatable?
Yes, adrenal cancer is treatable, especially if detected early. Surgery (adrenalectomy) is the most effective treatment for localized adrenal carcinoma, offering the potential for a cure. Advanced stages often require additional treatments such as mitotane therapy, chemotherapy, radiation, or emerging therapies like immunotherapy. While advanced adrenal carcinoma can be challenging to treat, ongoing research and clinical trials are improving outcomes.
How quickly does adrenal cancer spread?
Adrenal carcinoma is known to be aggressive and can spread quickly, especially in advanced stages. Metastasis often occurs to the liver, lungs, or lymph nodes. The rate of spread varies based on tumor biology, stage at diagnosis, and hormone-secreting activity. Early detection and prompt treatment are essential to slow progression and improve the patient’s prognosis.