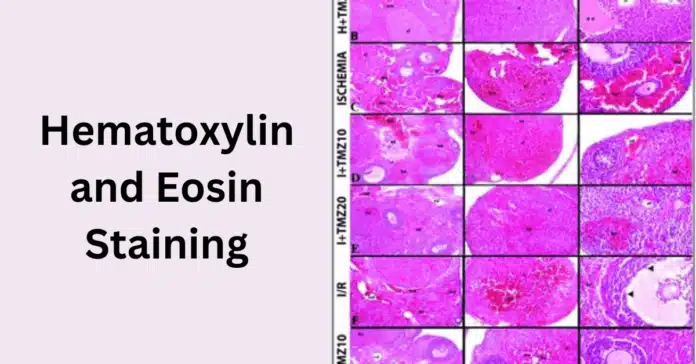
Hematoxylin and eosin staining is the most widely used staining technique in histology and pathology, providing essential insights into the microscopic structure of tissues. By staining the cell nuclei in blue-purple and the cytoplasm in pink, H&E staining allows pathologists to distinguish between different tissue components, making it a cornerstone in disease diagnosis, especially cancer. Its simplicity, reliability, and diagnostic value have made it an indispensable tool in medical research and clinical practice.
In this blog post, we will explore what hematoxylin and eosin staining is, how it works, and why it is so crucial in histopathology. We’ll cover the step-by-step staining protocol, discuss its applications in cancer diagnosis, and explain how to interpret stained tissue sections. Additionally, we’ll address common staining issues and introduce modern advancements and alternatives to H&E staining.
🔬 What is Hematoxylin and Eosin Staining?
Hematoxylin and eosin staining is a fundamental technique used in histology and pathology to visualize the microscopic structure of biological tissues. It is considered the gold standard for tissue staining because of its ability to clearly differentiate between various cellular components, allowing pathologists to detect abnormalities such as cancer, inflammation, and tissue damage.
The technique involves two dyes: hematoxylin and eosin, which stain specific parts of the cell differently. Hematoxylin is a basic dye that binds to acidic structures, primarily staining the nuclei of cells a blue or purple color. This highlights the genetic material (DNA) and nuclear details essential for identifying cellular abnormalities. On the other hand, eosin is an acidic dye that stains the cytoplasm and extracellular matrix a pink or red color. This contrast between the nucleus and cytoplasm provides a clear view of the tissue’s overall structure and organization.
H&E staining is widely used because it offers a balance between simplicity and diagnostic value. It provides essential information on:
- Cell morphology: The shape, size, and organization of cells.
- Tissue architecture: The arrangement of cells within tissues and organs.
- Pathological changes: Abnormalities such as tumors, necrosis, or fibrosis.
This staining method plays a crucial role in diagnosing a variety of diseases, particularly cancer, by revealing how cells and tissues are altered. It also serves as a foundational step before more specialized staining techniques, such as immunohistochemistry (IHC) or molecular pathology analyses.
In the following sections, we will dive deeper into how hematoxylin and eosin function in tissue staining, walk through the step-by-step staining protocol, discuss its applications in histopathology, and explore how to interpret H&E-stained tissue sections.
🔬 The Role of Hematoxylin and Eosin in Tissue Staining
Hematoxylin and eosin (H&E) staining plays a crucial role in histological analysis by providing clear contrast between different cellular structures, making it easier to observe tissue architecture and identify pathological changes. Each component of the stain has a specific function that contributes to the overall visualization of the tissue under a microscope.
📘 Hematoxylin: Staining the Nucleus
Hematoxylin is a basic dye that stains acidic structures, particularly the cell nucleus, blue to purple. The nucleus contains DNA and RNA, which are negatively charged (basophilic), allowing hematoxylin to bind effectively. This staining is essential for observing nuclear morphology, such as the shape, size, and chromatin patterns, which are critical for identifying cancerous changes and other pathological conditions.
The staining process with hematoxylin is often followed by a bluing step, where reagents like ammonia water or lithium carbonate are used to change the soluble hematoxylin into an insoluble blue form. This step enhances the contrast and clarity of the nuclear staining.
🔑 Key points about hematoxylin:
- Highlights nuclear details essential for diagnosis.
- Indicates cellular activities like mitosis and apoptosis.
- Helps detect abnormalities in nuclear size and shape, often seen in cancer cells.
🌸 Eosin: Staining the Cytoplasm
Eosin is an acidic dye that stains basic (eosinophilic) components of the cell, such as the cytoplasm, muscle fibers, collagen, and red blood cells, in shades of pink to red. Eosin binds to proteins and other positively charged elements, providing a striking contrast to the blue-purple nuclei stained by hematoxylin.
This contrast is vital for assessing the overall structure of the tissue and the relationship between cells and the extracellular matrix. Changes in the cytoplasmic staining patterns can indicate conditions like necrosis, fibrosis, or other tissue damage.
🔑 Key points about eosin:
- Highlights the cytoplasmic structure and extracellular components.
- Provides context for interpreting nuclear abnormalities.
- Helps identify changes in tissue consistency and organization.
🎨 Why the Combination of Hematoxylin and Eosin Matters
The combination of hematoxylin and eosin in tissue staining offers a balanced view of cellular and tissue architecture. Hematoxylin stains the nucleus, providing information about genetic material and cellular function, while eosin highlights the cytoplasm and surrounding structures, offering insights into the overall tissue organization.
This dual-staining approach is especially important in cancer diagnosis, where both nuclear abnormalities (e.g., irregular shapes, increased mitotic figures) and changes in tissue architecture (e.g., invasion into surrounding tissues) are key indicators of malignancy.
In the next section, we’ll explore the step-by-step protocol for performing hematoxylin and eosin staining, including essential tips for achieving optimal results.
⚗️ Hematoxylin and Eosin Staining Protocol: Step-by-Step Guide
The Hematoxylin and Eosin (H&E) staining protocol is a standard procedure in histology and pathology laboratories, providing essential contrast for tissue examination under a microscope. This step-by-step guide outlines the entire process, from tissue preparation to slide mounting, ensuring high-quality and reproducible results.
🧪 Step 1: Tissue Preparation
Before staining, tissues are typically preserved and embedded to maintain their structure.
- Fixation: Tissues are fixed using formalin to preserve cellular details and prevent degradation.
- Paraffin Embedding: Fixed tissues are embedded in paraffin wax to provide support for sectioning.
- Sectioning: Thin sections (3–5 µm) are cut using a microtome and mounted on glass slides.
💧 Step 2: Deparaffinization and Rehydration
Since tissue sections are embedded in paraffin, the wax must be removed before staining.
- Place slides in xylene to dissolve the paraffin.
- Rehydrate the tissue by passing the slides through a series of graded alcohol solutions (100%, 95%, 70%) and finally into distilled water.
🔍 Purpose: This step ensures that tissues are properly prepared to absorb aqueous staining solutions.
🔵 Step 3: Hematoxylin Staining (Nucleus Staining)
- Immerse slides in hematoxylin solution for 5–10 minutes.
- Rinse the slides in running tap water to remove excess stain.
- Perform the bluing step by immersing slides in ammonia water or lithium carbonate solution for 30 seconds to 1 minute.
- Rinse again in running water.
🔑 Purpose: Hematoxylin stains the nuclei blue-purple, highlighting nuclear details crucial for diagnosing pathological conditions.
🌊 Step 4: Differentiation (Optional)
- If the nuclear staining is too intense, briefly dip the slides in an acid alcohol solution to differentiate and remove excess hematoxylin.
- Rinse with tap water to stop the differentiation process.
🔍 Purpose: Ensures precise nuclear staining by reducing background coloration.
🌸 Step 5: Eosin Staining (Cytoplasm Staining)
- Immerse the slides in eosin solution for 1–3 minutes.
- Rinse briefly in distilled water.
🔑 Purpose: Eosin stains the cytoplasm, muscle fibers, and extracellular matrix in shades of pink, providing contrast to the blue-stained nuclei.
🌬️ Step 6: Dehydration and Clearing
- Pass the slides through graded alcohol solutions (70%, 95%, 100%) to remove water.
- Clear the tissue sections by immersing them in xylene, which makes the tissue transparent.
🔍 Purpose: Dehydration and clearing prepare the slides for permanent mounting, ensuring long-term preservation.
🩹 Step 7: Mounting the Slides
- Apply a few drops of mounting medium (e.g., DPX) on the tissue section.
- Carefully place a cover slip over the section, avoiding air bubbles.
🔑 Purpose: The mounting step protects the stained tissue and enhances visibility under a light microscope.
📝 Final Quality Check
- Examine the slides under a microscope to ensure optimal staining quality.
- Adjust staining times or reagents if the staining appears too faint or too intense.
💡 Tips for Optimal H&E Staining Results:
- Always use fresh reagents and solutions.
- Standardize staining times to maintain consistency between samples.
- Ensure proper fixation of tissues to avoid artifacts.
- Perform troubleshooting for issues such as overstaining, uneven staining, or faint coloration.
In the next section, we will explore the applications of H&E staining in histopathology, highlighting its importance in diagnosing various diseases, particularly cancer.
🏥 Applications of H&E Staining in Histopathology
Hematoxylin and eosin (H&E) staining plays a vital role in histopathology, the branch of pathology focused on the microscopic examination of tissue to study the manifestations of disease. As the gold standard in tissue staining, H&E provides essential insights into cellular and tissue structures, helping pathologists identify abnormalities, assess disease progression, and guide clinical decisions.
🩸 1. Cancer Diagnosis and Classification
H&E staining is indispensable in identifying and classifying various types of cancers.
- Tumor Identification: By highlighting differences in tissue architecture, H&E staining helps detect tumor margins and invasion patterns.
- Grading and Staging: It allows the evaluation of tumor grade by analyzing nuclear features, mitotic activity, and cellular differentiation—crucial factors for prognosis and treatment planning.
- Histological Subtyping: Specific cancer types, such as adenocarcinomas, squamous cell carcinomas, or lymphomas, exhibit unique histological features visible with H&E staining.
🔍 Example: In bladder cancer, H&E staining helps differentiate between non-muscle-invasive and muscle-invasive tumors based on how deeply the cancer cells penetrate the bladder wall.
🧬 2. Identifying Inflammatory and Infectious Diseases
H&E staining helps distinguish between acute and chronic inflammation by revealing changes in cellular infiltrates and tissue structure.
- Acute Inflammation: Characterized by the presence of neutrophils.
- Chronic Inflammation: Marked by lymphocytes, macrophages, and fibrosis.
- Infections: H&E can detect tissue responses to bacterial, viral, fungal, or parasitic infections by showing characteristic cellular patterns and damage.
🫀 3. Diagnosing Degenerative Diseases
H&E staining reveals degenerative changes in tissues that can indicate diseases such as:
- Liver cirrhosis: Shows fibrosis and regenerative nodules.
- Kidney disease: Highlights glomerular damage and tubular atrophy.
- Neurodegenerative disorders: Demonstrates neuronal loss and gliosis in brain tissues.
🩻 4. Evaluating Surgical Margins
After tumor removal, pathologists use H&E staining to check if the surgical margins are free of cancer cells.
- Negative margins: Indicate that no cancer cells are present at the edge of the removed tissue, suggesting complete tumor removal.
- Positive margins: Suggest that cancerous tissue remains, requiring further treatment.
🧫 5. Assessing Tissue Architecture and Cellular Morphology
H&E staining provides clear visualization of tissue architecture, allowing pathologists to:
- Identify necrosis, fibrosis, and vascular abnormalities.
- Examine cellular morphology, including nuclear size, shape, and chromatin patterns, which are essential for diagnosing malignancies.
- Evaluate tissue organization, which can be disrupted in diseases such as cancer or fibrosis.
🧪 6. Supporting Immunohistochemistry (IHC) and Molecular Studies
H&E-stained slides often serve as a reference for more advanced diagnostic techniques.
- Immunohistochemistry (IHC): H&E staining helps select appropriate tissue areas for further analysis using specific antibodies.
- Molecular Pathology: Techniques like PCR, FISH, and next-generation sequencing rely on well-characterized tissue samples, for which H&E staining provides foundational morphological insights.
🌿 7. Research and Educational Applications
- In cancer research, H&E staining is used to study tumor development, progression, and response to therapies.
- In medical education, it remains a fundamental tool for teaching histological and pathological concepts to students.
🏹 Why H&E Staining Remains Indispensable
H&E staining remains the cornerstone of histopathology due to its ability to:
- Provide rapid and cost-effective results.
- Offer comprehensive information on tissue structure and cellular morphology.
- Support other diagnostic methods by guiding advanced molecular and immunological analyses.
In the next section, we’ll discuss how to interpret H&E-stained tissue sections, focusing on key histological features and what they reveal about normal and pathological conditions.
🔬 Interpretation of Hematoxylin and Eosin-Stained Tissue Sections
Interpreting Hematoxylin and Eosin (H&E)-stained tissue sections is a fundamental skill in histopathology, allowing pathologists to distinguish between normal and pathological tissues.
📌 1. Identifying Normal Tissue Architecture
H&E staining provides contrast between different cellular and extracellular components:
- Nuclei: Stained blue to purple by hematoxylin, allowing assessment of size, shape, chromatin distribution, and mitotic figures.
- Cytoplasm: Stained pink to red by eosin, helping differentiate cell types and structures.
- Extracellular Matrix (ECM): Collagen, muscle fibers, and connective tissues appear in varying shades of pink, helping assess structural integrity.
🔍 Example: In normal epithelial tissues, nuclei appear evenly spaced with a uniform chromatin pattern, while the cytoplasm maintains a consistent eosinophilic tone.
🚨 2. Recognizing Pathological Changes
H&E staining is key to identifying abnormal histological features that indicate disease.
A. Nuclear Abnormalities (Indicators of Malignancy)
- Nuclear Enlargement (Anisokaryosis): Irregularly large nuclei suggest rapid cell proliferation, often seen in cancerous tissues.
- Hyperchromasia: Dark-staining nuclei due to increased DNA content, common in malignancies.
- Irregular Nuclear Borders: Indicative of dysplasia or invasive carcinoma.
- Increased Mitotic Figures: A higher number of dividing cells suggests aggressive tumor growth.
🔍 Example: In bladder cancer, tumor cells often exhibit enlarged, hyperchromatic nuclei with prominent nucleoli, indicating malignancy.
B. Cytoplasmic Changes
- Eosinophilia (Increased Pink Staining): Seen in necrosis, muscle cells, or apoptotic cells.
- Pale or Vacuolated Cytoplasm: Suggests fatty degeneration, mucin production, or glycogen accumulation.
- Granular Cytoplasm: Indicates inflammatory or metabolic conditions.
🔍 Example: In liver cirrhosis, hepatocytes may exhibit vacuolated cytoplasm due to fat accumulation, known as steatosis.
C. Tissue Architecture Disruptions
- Loss of Polarity: Cells lose their organized structure, seen in high-grade dysplasia and cancerous tissues.
- Necrosis: Dead cells appear eosinophilic with pyknotic (shrunken) or fragmented nuclei.
- Fibrosis: Excess collagen deposition in chronic inflammation appears intensely eosinophilic.
🔍 Example: In chronic kidney disease, glomerular fibrosis and tubular atrophy lead to disrupted tissue organization.
🔥 3. Detecting Inflammation and Infection
H&E staining helps differentiate between acute and chronic inflammation based on cellular infiltration.
- Acute Inflammation: Presence of neutrophils with multi-lobed nuclei and eosinophilic cytoplasm.
- Chronic Inflammation: Dominated by lymphocytes (small dark nuclei) and macrophages.
- Granulomas: Aggregates of macrophages surrounded by lymphocytes, seen in tuberculosis and sarcoidosis.
🔍 Example: In bacterial infections, neutrophils cluster around infected tissues, while in viral infections, lymphocytes dominate.
🏥 4. Identifying Tissue-Specific Pathologies
Different tissues exhibit characteristic staining patterns in disease states:
- Liver: Fat accumulation (steatosis), fibrosis (cirrhosis), and necrosis.
- Lung: Inflammatory infiltrates in pneumonia, fibrosis in interstitial lung diseases.
- Breast: Architectural distortion in ductal carcinoma, fibrosis in sclerosing adenosis.
🔍 Example: In lung cancer, a disrupted alveolar structure with pleomorphic tumor cells suggests malignancy.
In the next section, we’ll explore common artifacts in H&E staining and troubleshooting techniques to ensure high-quality histological analysis.
🛠️ Troubleshooting Common H&E Staining Issues
Even though Hematoxylin and Eosin (H&E) staining is considered the gold standard in histopathology, various technical issues can arise during the process. These issues can affect the quality and accuracy of tissue interpretation. Proper troubleshooting ensures clear, precise staining results, which are critical for accurate diagnosis.
⚡ 1. Weak Hematoxylin Staining (Pale Nuclei)
🔎 Problem:
Nuclei appear faint or poorly defined, making it difficult to assess nuclear morphology.
🛠️ Causes:
- Under-staining in hematoxylin.
- Over-differentiation during acid alcohol steps.
- Hematoxylin reagent degradation.
💡 Solutions:
- Increase hematoxylin staining time.
- Reduce differentiation time or acid alcohol concentration.
- Use fresh hematoxylin solution or filter it to remove precipitates.
- Check pH and temperature of water used in washing steps.
💧 2. Excessive Hematoxylin Staining (Dark or Smudged Nuclei)
🔎 Problem:
Nuclei are too dark, obscuring chromatin patterns.
🛠️ Causes:
- Over-staining with hematoxylin.
- Incomplete differentiation step.
💡 Solutions:
- Shorten hematoxylin staining time.
- Perform proper differentiation using acid alcohol until desired nuclear clarity is achieved.
- Ensure proper timing during bluing step to neutralize excess stain.
🎨 3. Weak Eosin Staining (Pale Cytoplasm)
🔎 Problem:
Cytoplasm and extracellular components appear faint or poorly contrasted.
🛠️ Causes:
- Under-staining in eosin.
- Over-washing after eosin staining.
- Eosin solution degradation.
💡 Solutions:
- Increase eosin staining time.
- Reduce washing time after eosin application.
- Use fresh eosin and adjust pH (optimal: 4.5–5).
⚠️ 4. Excessive Eosin Staining (Overstained Cytoplasm)
🔎 Problem:
Cytoplasm appears overly bright pink, obscuring tissue details.
🛠️ Causes:
- Over-staining in eosin.
- Inadequate differentiation or washing steps.
💡 Solutions:
- Decrease eosin staining time.
- Increase washing time in ethanol after eosin staining.
- Adjust pH of eosin solution if needed.
🌫️ 5. Background Staining (Non-Specific Staining)
🔎 Problem:
Diffuse staining makes distinguishing cellular components difficult.
🛠️ Causes:
- Incomplete dehydration and clearing.
- Residual paraffin in tissue.
- Contaminated staining reagents.
💡 Solutions:
- Ensure complete deparaffinization using fresh xylene.
- Use fresh, filtered reagents.
- Adjust dehydration times in ethanol series.
🔍 6. Incomplete Deparaffinization (Hazy or Cloudy Appearance)
🔎 Problem:
Tissue appears hazy, affecting clarity.
🛠️ Causes:
- Insufficient xylene exposure.
- Thick tissue sections.
💡 Solutions:
- Extend deparaffinization time in xylene.
- Use thinner tissue sections (4–5 µm recommended).
- Check xylene purity and replace if necessary.
🌈 7. Uneven Staining (Patchy or Blotchy Appearance)
🔎 Problem:
Irregular staining patterns across the tissue section.
🛠️ Causes:
- Incomplete reagent penetration.
- Uneven drying of slides before staining.
- Air bubbles during mounting.
💡 Solutions:
- Ensure uniform drying of tissue sections before staining.
- Avoid air bubbles during mounting.
- Regularly change staining solutions to maintain consistency.
🏞️ 8. Staining Artifacts (False Patterns in Tissue)
🔎 Problem:
Artifacts can mimic pathological features, leading to misinterpretation.
🛠️ Common Artifacts and Solutions:
- Folding of Tissue Sections: Use proper microtomy techniques and ensure flat sections.
- Knife Marks: Sharpen or replace microtome blades.
- Water Bubbles: Remove bubbles before coverslipping; use appropriate mounting medium.
- Precipitation of Stains: Filter hematoxylin and eosin solutions regularly.
💎 9. Bluing Issues (Nuclei Not Properly Bluish)
🔎 Problem:
Nuclei may remain reddish or purplish due to inadequate bluing.
🛠️ Causes:
- Incorrect bluing reagent or time.
- Inadequate washing after hematoxylin staining.
💡 Solutions:
- Use appropriate bluing reagent (e.g., ammonium hydroxide solution).
- Increase bluing time to ensure complete color development.
Conclusion
Hematoxylin and Eosin (H&E) staining remains an indispensable technique in histopathology, providing clear visualization of tissue architecture and cellular details essential for accurate diagnosis. From understanding its principles and protocols to interpreting stained sections and troubleshooting common issues, mastering H&E staining is crucial for both clinical and research applications. By following proper staining procedures and addressing potential challenges, high-quality, reliable results can be consistently achieved, ultimately contributing to better disease diagnosis and patient care.