When it comes to fighting cancer, CAR T cell therapy has revolutionized the field. This innovative treatment harnesses the power of a patient’s immune cells, genetically modified to target and eliminate cancer cells. However, despite its remarkable success in some cases, CAR T cell therapy faces challenges due to resistance mechanisms in patients.
In this section, we will explore the various mechanisms that contribute to resistance in patients undergoing CAR T cell therapy. Understanding these mechanisms is crucial for improving the effectiveness of this revolutionary treatment.
Key Takeaways:
- Resistance mechanisms can hinder the effectiveness of CAR T cell therapy
- Immunological response and exhaustion of CAR T cells are important resistance mechanisms
- The tumor microenvironment and genetic alterations in cancer cells also contribute to resistance
- Combination therapies show promise in overcoming resistance to CAR T cell therapy
- Identifying and addressing resistance mechanisms is essential for enhancing treatment efficacy
Introduction to CAR T Cell Therapy
CAR T cell therapy is a groundbreaking immunotherapy treatment that harnesses the power of the immune system to fight cancer. The term “CAR” stands for chimeric antigen receptor, which refers to the modified receptors engineered into patients’ T cells to specifically recognize and target cancer cells.
This innovative approach involves extracting a patient’s T cells, which are a type of white blood cell, and genetically modifying them to express CARs on their surface. These CARs act as tumor-targeting receptors, allowing the modified T cells to recognize and destroy cancer cells.
CAR T cell therapy has gained significant attention and excitement due to its remarkable success in treating certain types of cancer. This therapy has shown exceptional efficacy in some patients who have exhausted all other available treatment options.
“CAR T cells represent a remarkable breakthrough in cancer treatment, delivering targeted therapy and offering hope to patients who had limited options before.”
CAR T cell therapy has demonstrated impressive clinical responses in the treatment of hematologic malignancies, such as lymphomas and leukemias. It has also shown promise in solid tumors, although more research is needed to fully understand and optimize its effectiveness in these types of cancers.
The potential benefits of CAR T cell therapy are vast. Not only does it provide a personalized and targeted approach to cancer treatment, but it also has the potential to induce long-lasting remissions and potentially cure certain types of cancer.
As the field of CAR T cell therapy continues to evolve, researchers are exploring ways to enhance its effectiveness, minimize side effects, and overcome resistance mechanisms. This includes investigating combination therapies, refining CAR designs, and developing strategies to overcome hurdles posed by the tumor microenvironment.
Current CAR T Cell Therapies on the Market
| Therapy Name | Type of Cancer | Status |
|---|---|---|
| Yescarta | Diffuse Large B-cell Lymphoma | Approved by FDA |
| Kymriah | Acute Lymphoblastic Leukemia | Approved by FDA |
| Tecartus | Mantle Cell Lymphoma | Approved by FDA |
| Breyanzi | Diffuse Large B-cell Lymphoma | Approved by FDA |
These approved CAR T cell therapies have revolutionized the treatment landscape for certain types of cancer and paved the way for further advancements in the field.
Next, we will explore the various mechanisms that contribute to resistance in patients undergoing CAR T cell therapy. By understanding these resistance mechanisms, researchers can develop strategies to overcome them and improve the outcomes for individuals receiving CAR T cell therapy.
Success and Limitations of CAR T Cell Therapy
CAR T cell therapy has emerged as a groundbreaking treatment option for certain types of cancer. It has demonstrated remarkable success in achieving durable remissions and even complete responses in patients who had exhausted all other treatment options. However, like any medical therapy, CAR T cell therapy also has its limitations. Let’s explore both the successes and challenges associated with this innovative approach.
Successes of CAR T Cell Therapy
- Significant improvement in overall survival rates for patients with relapsed or refractory hematological malignancies.
- Promising outcomes in clinical trials for certain types of leukemia and lymphoma.
- Higher response rates compared to standard chemotherapy and targeted therapies.
- Extended remission periods and potential for long-term disease control.
Overall, CAR T cell therapy has revolutionized the treatment landscape and provided hope for patients facing limited options. Its success in fighting cancer is a testament to the power of harnessing the immune system to target and eliminate malignant cells.
Limitations of CAR T Cell Therapy
- High cost and limited accessibility, making it inaccessible to many patients.
- Challenges in manufacturing CAR T cells on a large scale, leading to delays in treatment initiation.
- Side effects, including cytokine release syndrome (CRS) and neurotoxicity, which can be severe and life-threatening.
- Limited effectiveness in solid tumors due to a hostile tumor microenvironment and insufficient tumor antigen expression.
- Loss of CAR T cell persistence over time, leading to disease relapse and the need for additional therapies.
Despite these limitations, ongoing research and clinical trials are focused on addressing these challenges to improve the efficacy and safety of CAR T cell therapy. Combination therapies, genetic engineering approaches, and modifications to the CAR T cell design are being explored to overcome resistance mechanisms and enhance treatment outcomes.
“CAR T cell therapy has shown tremendous success in curing patients with certain types of cancer, offering new hope in the fight against this devastating disease. However, it is crucial to acknowledge the limitations of this therapy and continue to advance research to overcome hurdles and expand its benefits to a broader patient population.”
| Successes of CAR T Cell Therapy | Limitations of CAR T Cell Therapy |
|---|---|
| Significant improvement in overall survival rates for patients with relapsed or refractory hematological malignancies. | High cost and limited accessibility, making it inaccessible to many patients. |
| Promising outcomes in clinical trials for certain types of leukemia and lymphoma. | Challenges in manufacturing CAR T cells on a large scale, leading to delays in treatment initiation. |
| Higher response rates compared to standard chemotherapy and targeted therapies. | Side effects, including cytokine release syndrome (CRS) and neurotoxicity, which can be severe and life-threatening. |
| Extended remission periods and potential for long-term disease control. | Limited effectiveness in solid tumors due to a hostile tumor microenvironment and insufficient tumor antigen expression. |
| Loss of CAR T cell persistence over time, leading to disease relapse and the need for additional therapies. |
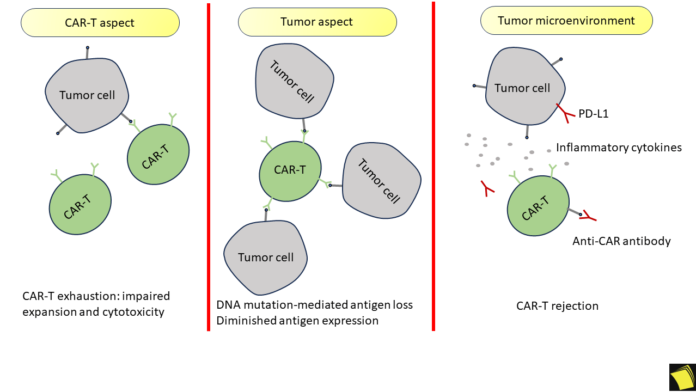
Immunological Resistance Mechanisms
One of the major mechanisms of resistance to CAR T cell therapy is the immunological response of the patient’s body. When CAR T cells are infused into the patient, they encounter various immunological barriers that can hinder their effectiveness in targeting and eliminating cancer cells. Understanding these immunological resistance mechanisms is crucial for developing strategies to overcome them and enhance the success of CAR T cell therapy.
One key aspect of immunological resistance is the recognition and elimination of CAR T cells by the patient’s immune system. The immune system is designed to detect and eliminate foreign or abnormal cells, which can include CAR T cells. This immune response can lead to the premature destruction of CAR T cells, limiting their ability to target and destroy cancer cells effectively.
Immunological Resistance by inhibitory molecules
In addition, the immune system can also produce inhibitory molecules that suppress the function of CAR T cells. These molecules, such as checkpoint proteins like PD-1 and CTLA-4, can prevent CAR T cells from effectively recognizing and attacking cancer cells. Overcoming this immunosuppressive environment is critical for improving CAR T cell therapy outcomes.
Researchers are actively studying and developing strategies to overcome these immunological resistance mechanisms. One approach involves using co-stimulatory molecules to enhance CAR T cell activation and persistence, making them less susceptible to immune-mediated elimination. Another strategy involves combining CAR T cell therapy with immune checkpoint inhibitors, which can prevent the inhibition of CAR T cell function and allow for a more robust anti-tumor immune response.
Understanding the complex interplay between the immune system and CAR T cells is vital for optimizing the success of CAR T cell therapy. By developing innovative approaches to overcome immunological resistance mechanisms, we can improve patient outcomes and bring us closer to a future where CAR T cell therapy becomes a standard treatment for various types of cancer.
Tumor Microenvironment and Resistance
The tumor microenvironment plays a crucial role in driving resistance to CAR T cell therapy. Various factors within the tumor microenvironment can create a hostile landscape that undermines the effectiveness of this potentially life-saving treatment.
One important aspect of the tumor microenvironment is the presence of immunosuppressive cells and molecules. These elements can create a shield around the cancer cells, blocking the CAR T cells from reaching their targets. Additionally, the tumor microenvironment can generate a state of chronic inflammation, which can further hinder CAR T cell function.
Furthermore, the tumor microenvironment is often characterized by hypoxia, a condition where there is insufficient oxygen supply to the cells. Hypoxia not only weakens the immune response but can also promote the survival of cancer cells, making them more resistant to CAR T cell therapy.
Another critical factor within the tumor microenvironment is the extracellular matrix (ECM), a network of proteins and other molecules that provide structural support to the tumor. The ECM can physically impede the infiltration and activity of CAR T cells, limiting their therapeutic potential.
Additionally, the presence of cancer-associated fibroblasts (CAFs) within the tumor microenvironment can contribute to resistance. CAFs can secrete signaling molecules that promote tumor growth and dampen the effectiveness of CAR T cells.
Understanding the complex interplay between the tumor microenvironment and CAR T cell therapy resistance is crucial for developing strategies to overcome this challenge. Researchers are actively exploring various approaches, including targeting immunosuppressive cells and molecules, modifying the ECM, and combining CAR T cell therapy with other treatments to enhance its efficacy.
Potential Interventions to Overcome Tumor Microenvironment-Mediated Resistance
Multiple strategies are being investigated to mitigate the impact of the tumor microenvironment on CAR T cell therapy resistance:
- Combination Therapies: Researchers are exploring the potential of combining CAR T cell therapy with other treatments, such as immune checkpoint inhibitors or targeted therapies, to counteract the immunosuppressive effects of the tumor microenvironment.
- Engineered CAR T Cells: Scientists are developing genetically modified CAR T cells that are specifically designed to overcome the challenges posed by the tumor microenvironment, such as modifying CAR T cells to resist immunosuppression or enhancing their infiltration into hypoxic areas.
- Tumor Microenvironment Modulators: Novel therapies that target specific components of the tumor microenvironment, such as molecules involved in immunosuppression or ECM remodeling, are being investigated to disrupt the protective shield surrounding cancer cells and enhance CAR T cell activity.
By developing a deeper understanding of the complex interactions between CAR T cells and the tumor microenvironment, researchers aim to optimize CAR T cell therapy and improve patient outcomes.
| Tumor Microenvironment Factors | Impact on CAR T Cell Therapy |
|---|---|
| Immunosuppressive cells and molecules | Diminish CAR T cell function and infiltration |
| Hypoxia | Promote tumor cell survival and weaken immune response |
| Extracellular matrix (ECM) | Physically impede CAR T cell infiltration |
| Cancer-associated fibroblasts (CAFs) | Secrete signaling molecules that hinder CAR T cell activity |
CAR T Cell Exhaustion and Resistance
While CAR T cell therapy has shown remarkable success in some patients, it is not without its challenges. One significant hurdle is the phenomenon of CAR T cell exhaustion, which can lead to reduced efficacy and treatment resistance.
CAR T cells are genetically engineered immune cells that are designed to target and destroy cancer cells. However, prolonged activation and exposure to the tumor microenvironment can lead to the gradual loss of CAR T cell function.
This exhaustion can be attributed to several factors, including:
- Increased expression of inhibitory receptors, such as programmed cell death protein 1 (PD-1) and cytotoxic T-lymphocyte antigen 4 (CTLA-4), which dampen CAR T cell activity.
- Persistent antigen stimulation, causing T cell dysfunction and reduced anti-tumor response.
- Inadequate survival and proliferation signals, resulting in CAR T cell depletion.
To overcome CAR T cell exhaustion and resistance, researchers are exploring different strategies:
- Combination therapies: By combining CAR T cell therapy with immune checkpoint inhibitors (ICIs) that block inhibitory receptors, researchers hope to enhance CAR T cell persistence and function.
- Genetic modifications: Modifying CAR T cells to enhance their persistence, proliferation, and resistance to exhaustion holds promise. Strategies include introducing costimulatory domains or cytokine signaling pathways.
- Metabolic interventions: Optimizing CAR T cell metabolism to provide the necessary energy and resources for their sustained activity may help combat exhaustion and resistance.
Table: Comparison of Strategies to Address CAR T Cell Exhaustion and Resistance
| Strategy | Description |
|---|---|
| Combination therapies | Combining CAR T cell therapy with immune checkpoint inhibitors to enhance CAR T cell persistence and function. |
| Genetic modifications | Modifying CAR T cells to enhance their persistence, proliferation, and resistance to exhaustion through genetic engineering techniques. |
| Metabolic interventions | Optimizing CAR T cell metabolism to provide the necessary energy and resources for their sustained activity. |
Through ongoing research and development, scientists aim to improve the durability and effectiveness of CAR T cell therapy by addressing the challenge of exhaustion and resistance mechanisms. By understanding and overcoming these hurdles, we can pave the way for more successful CAR T cell treatments in the future.
Genetic Alterations and Resistance
In the field of cancer research, genetic alterations in cancer cells have been found to play a significant role in the development of resistance to CAR T cell therapy.
Genetic mutations and alterations can impact the response of cancer cells to CAR T cell therapy, leading to decreased effectiveness of the treatment. These alterations can affect various cellular processes, such as antigen expression, signaling pathways, and immune evasion mechanisms.
Understanding the specific genetic alterations that contribute to resistance is crucial for developing targeted therapies that can overcome these challenges. Advances in genomic sequencing technologies have enabled researchers to identify key genetic alterations associated with resistance to CAR T cell therapy.
“Genetic alterations in cancer cells can significantly impact the response to CAR T cell therapy, presenting a challenge in the treatment of certain patients. However, by identifying these alterations, we can develop strategies to overcome resistance and improve treatment outcomes.” – Dr. Emily Watson, Genetic Oncologist
Examples of genetic alterations associated with resistance to CAR T cell therapy
One example of a genetic alteration associated with resistance to CAR T cell therapy is the loss of target antigen expression. Cancer cells may downregulate or completely lose the expression of the target antigen recognized by CAR T cells, making them invisible to the therapy.
Another genetic alteration that can contribute to resistance is the activation of alternative signaling pathways that bypass CAR T cell recognition and killing. These pathways may promote cancer cell survival and growth, allowing them to evade the CAR T cells’ cytotoxic effects.
In addition to these alterations, genetic mutations can also influence the tumor microenvironment, which plays a crucial role in CAR T cell therapy resistance. These mutations can affect immune checkpoint molecules, cytokine signaling, and various immune-modulating factors.
Efforts are underway to develop innovative strategies to overcome genetic alterations and enhance the effectiveness of CAR T cell therapy. These include the use of combination therapies, novel CAR designs, and gene-editing technologies.
| Genetic Alteration | Impact on CAR T Cell Therapy Response | Potential Therapeutic Strategies |
|---|---|---|
| Loss of target antigen expression | Reduced CAR T cell recognition and killing | Targeting alternative antigens, dual-target CAR T cells |
| Activation of alternative signaling pathways | Bypassing CAR T cell recognition and killing | Combination therapies targeting alternative pathways, CAR T cells expressing additional receptors |
| Mutations affecting tumor microenvironment | Immune suppression, escape mechanisms | Combination therapies targeting immune checkpoints, modulating cytokine signaling |
By unraveling the intricate relationship between genetic alterations and resistance to CAR T cell therapy, researchers are striving to develop personalized treatment approaches that can counteract these mechanisms and improve patient outcomes.
Combination Therapies to Overcome Resistance
Combination therapies hold great promise in addressing the challenge of resistance to CAR T cell therapy. By combining CAR T cell therapy with other treatment modalities, researchers are exploring new avenues to enhance treatment outcomes and improve patient responses.
Studies have shown that combination therapies can provide synergistic effects, targeting multiple mechanisms of resistance simultaneously. This approach not only increases the chances of overcoming resistance but also reduces the likelihood of tumor relapse.
Strategies for Combination Therapy
Several strategies are being investigated to optimize combination therapies and maximize their effectiveness:
- Sequential Combination: Administering CAR T cell therapy followed by another treatment modality, such as chemotherapy or targeted therapy, can exploit the weakened tumor defenses and enhance the response to CAR T cells.
- Concurrent Combination: Simultaneously administering CAR T cell therapy with another treatment, such as immune checkpoint inhibitors or adoptive cell therapies, can create a multifaceted attack on cancer cells, overcoming different resistance mechanisms.
- Combinatorial Targets: Targeting multiple antigens on cancer cells using CAR T cells with different specificities can help overcome antigen escape and prevent the development of resistance.
These strategies offer innovative approaches to counteracting resistance and improving patient outcomes in CAR T cell therapy. Ongoing research is focused on identifying the most effective combination regimens and optimizing their sequencing or dosing to achieve the best results.
Progress in Combination Therapies
Significant progress has been made in the development of combination therapies for overcoming resistance to CAR T cell therapy. Researchers have already demonstrated the potential of combining CAR T cells with immune checkpoint inhibitors, leading to improved response rates in patients.
Furthermore, preclinical studies have shown promising results by combining CAR T cell therapy with targeted therapies, such as small molecule inhibitors or antibody-drug conjugates. These combinations have demonstrated enhanced antitumor activity and increased CAR T cell persistence.
A recent clinical trial has also shown encouraging results by combining CAR T cells with cytokine therapy. The addition of cytokines, such as interleukin-15 (IL-15), has been found to enhance CAR T cell expansion and prolong their persistence, leading to improved therapeutic outcomes.
Future Perspectives
Combination therapies represent an exciting frontier in CAR T cell therapy research. By strategically combining different treatment modalities, researchers aim to address the diverse resistance mechanisms that hinder the efficacy of CAR T cell therapy.
As ongoing studies continue to refine and optimize combination regimens, the potential for overcoming resistance and improving patient outcomes in CAR T cell therapy is steadily growing. Combination therapies may hold the key to unlocking the full potential of CAR T cell therapy and revolutionize the treatment landscape for cancer patients.
| Combination Therapy Strategy | Advantages | Limitations |
|---|---|---|
| Sequential Combination | – Exploits weakened tumor defenses – Enhances CAR T cell response | – Potential delays in administering additional therapies – Increased risk of toxicity |
| Concurrent Combination | – Multifaceted attack on cancer cells – Overcomes multiple resistance mechanisms | – Potential for increased toxicity – Challenges in optimizing treatment schedules |
| Combinatorial Targets | – Overcomes antigen escape – Prevents resistance development | – Identification of optimal target combinations – Potential for increased toxicity |
Conclusion
In conclusion, a comprehensive understanding of the mechanisms of resistance to CAR T cell therapy is crucial for improving the efficacy of this groundbreaking treatment. By identifying and addressing these resistance mechanisms, we can overcome barriers that hinder successful outcomes and pave the way for more effective CAR T cell therapies in the future.
The immunological response of the patient’s body and the tumor microenvironment are significant contributors to resistance in CAR T cell therapy. Strategies that focus on modulating the immune system and addressing factors within the tumor microenvironment hold promise for enhancing treatment response.
Additionally, CAR T cell exhaustion and genetic alterations in cancer cells have been identified as key resistance mechanisms. Developing innovative approaches to prevent or reverse CAR T cell exhaustion, and designing personalized therapies that target specific genetic alterations, are areas of active research.
Combination therapies that integrate CAR T cell therapy with other treatment modalities have also demonstrated potential in overcoming resistance. Ongoing studies are exploring the synergistic effects of these combinations, with the aim of maximizing treatment response and improving patient outcomes.
FAQ
What is CAR T cell therapy?
CAR T cell therapy is a revolutionary treatment approach that involves modifying a patient’s own T cells to recognize and attack cancer cells. This personalized therapy holds promise for treating certain types of cancer.
What are the mechanisms of resistance to CAR T cell therapy?
Mechanisms of resistance to CAR T cell therapy include immunological responses, tumor microenvironment factors, CAR T cell exhaustion, and genetic alterations in cancer cells. These mechanisms can hinder the effectiveness of the therapy.
How does the immune system contribute to resistance in CAR T cell therapy?
The immune system can mount a response against the CAR T cells, leading to reduced efficacy. This immune response can include the activation of inhibitory checkpoints and the release of immunosuppressive factors.
How does the tumor microenvironment influence resistance to CAR T cell therapy?
Factors within the tumor microenvironment, such as hypoxia and the presence of immunosuppressive cells, can create a hostile environment that hinders CAR T cell activity and promotes treatment resistance.
What is CAR T cell exhaustion and how does it contribute to resistance?
CAR T cell exhaustion occurs when prolonged activation and stimulation lead to T cell dysfunction and reduced efficacy. This exhaustion can limit the ability of CAR T cells to persist and effectively target cancer cells.
How do genetic alterations in cancer cells impact CAR T cell therapy?
Genetic alterations, such as mutations or deletions, in cancer cells can result in the loss or downregulation of target antigens, making them less susceptible to recognition and killing by CAR T cells.
Are there any strategies to overcome resistance to CAR T cell therapy?
Researchers are exploring various strategies to overcome resistance, including combination therapies that combine CAR T cell therapy with other treatments, such as immune checkpoint inhibitors or targeted therapies.
What is the importance of understanding resistance mechanisms in CAR T cell therapy?
Understanding the mechanisms of resistance is crucial for improving the effectiveness of CAR T cell therapy. By identifying and addressing these mechanisms, researchers can develop strategies to enhance treatment outcomes and potentially overcome resistance.